-
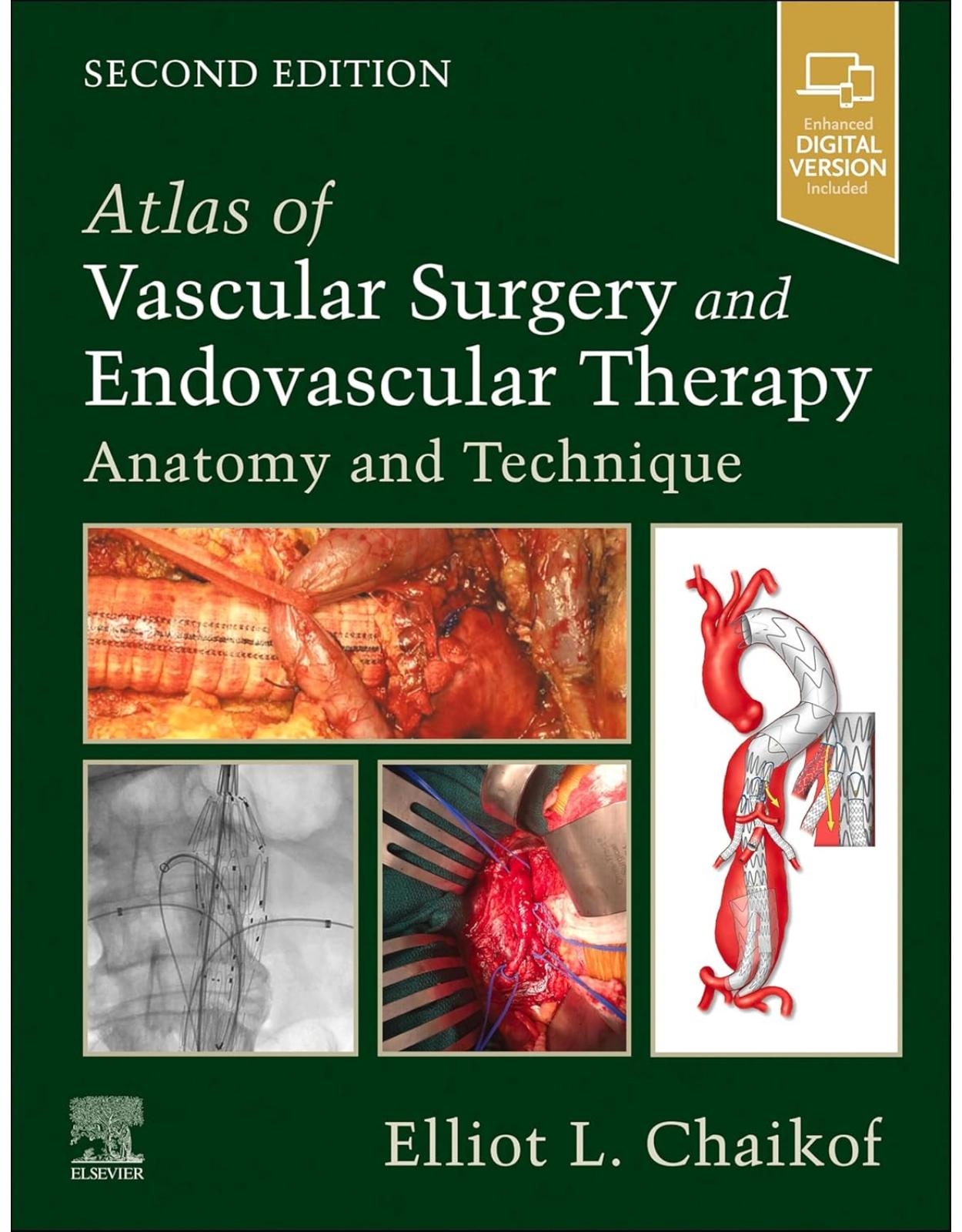
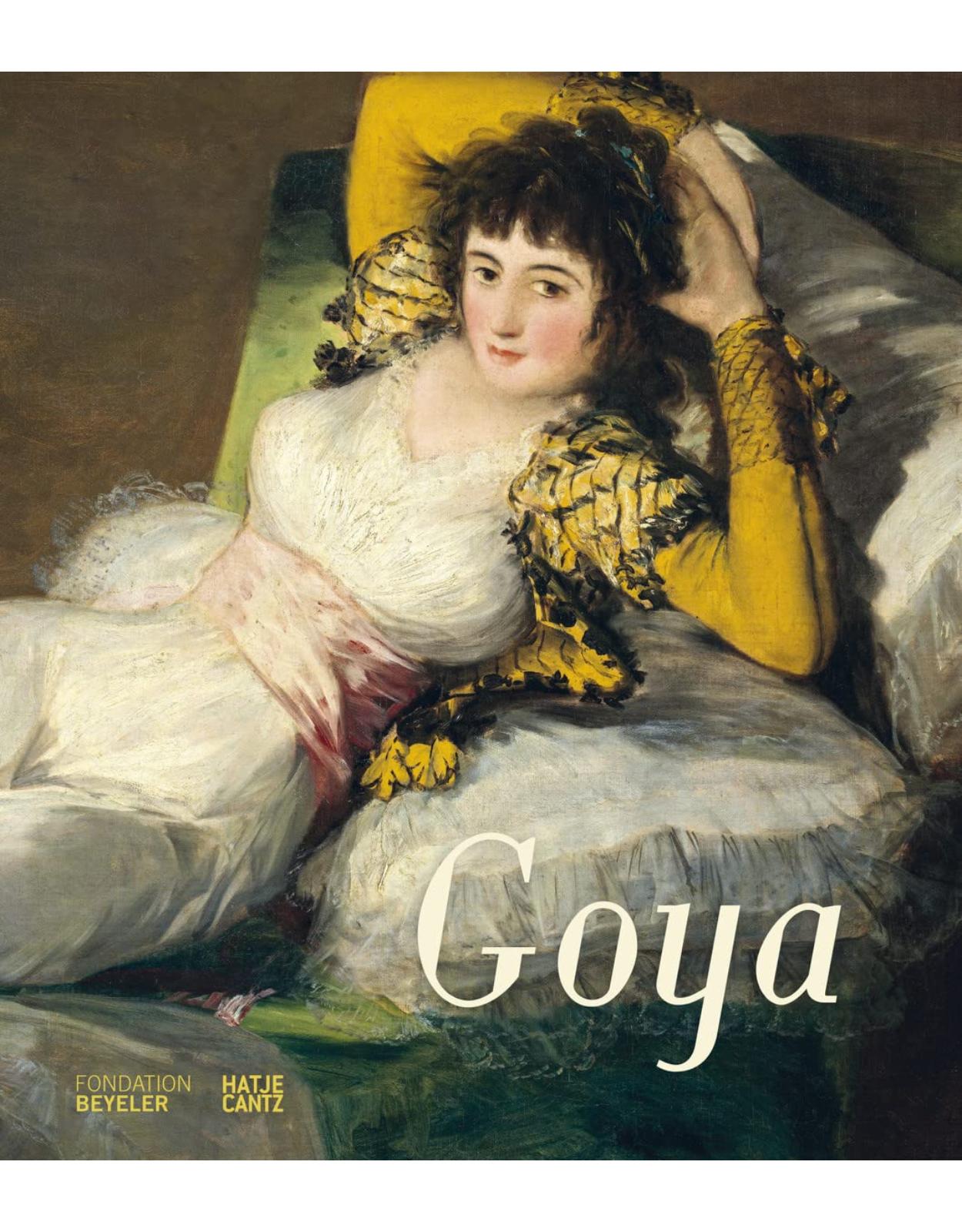
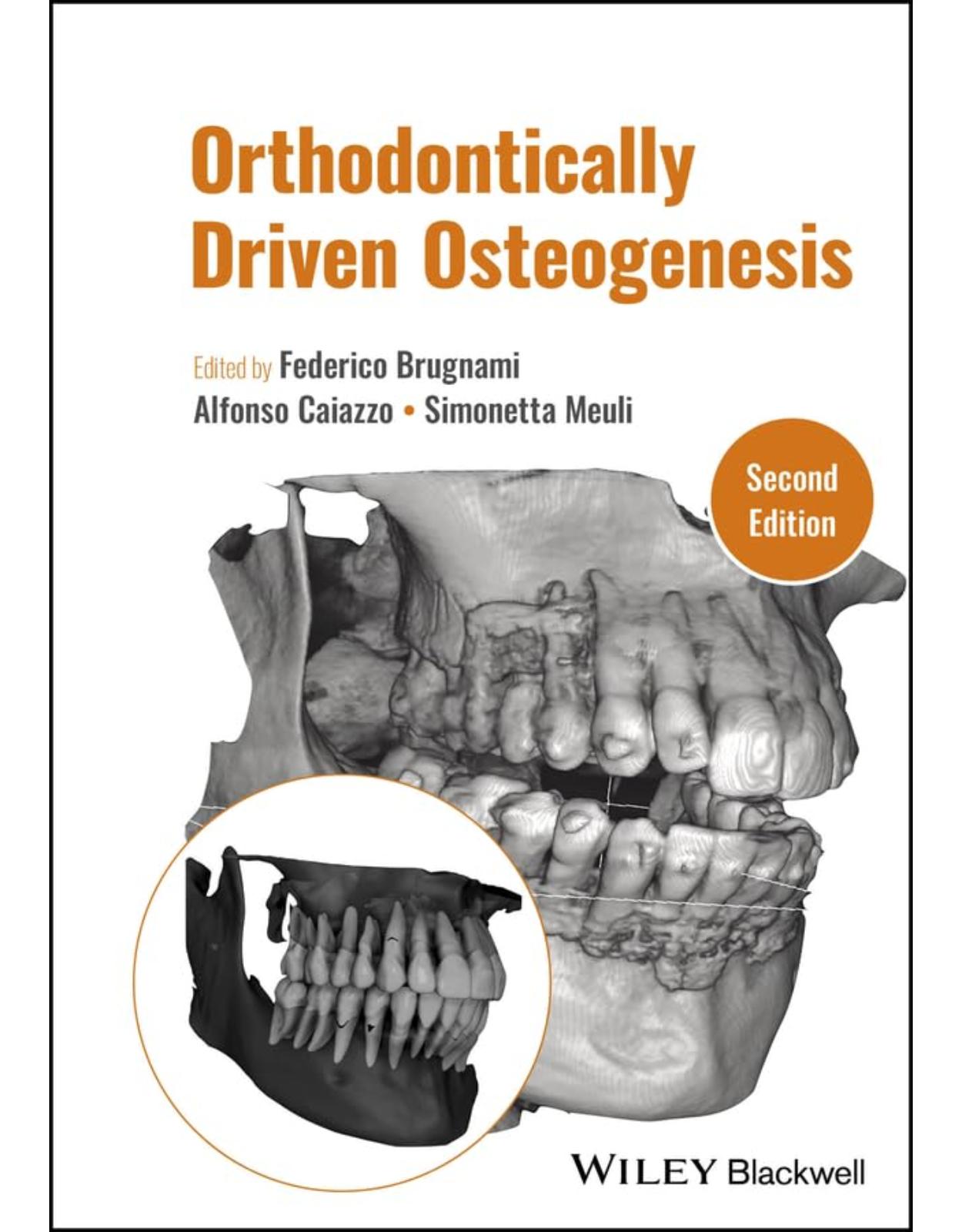
41000 lei 37000 lei
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
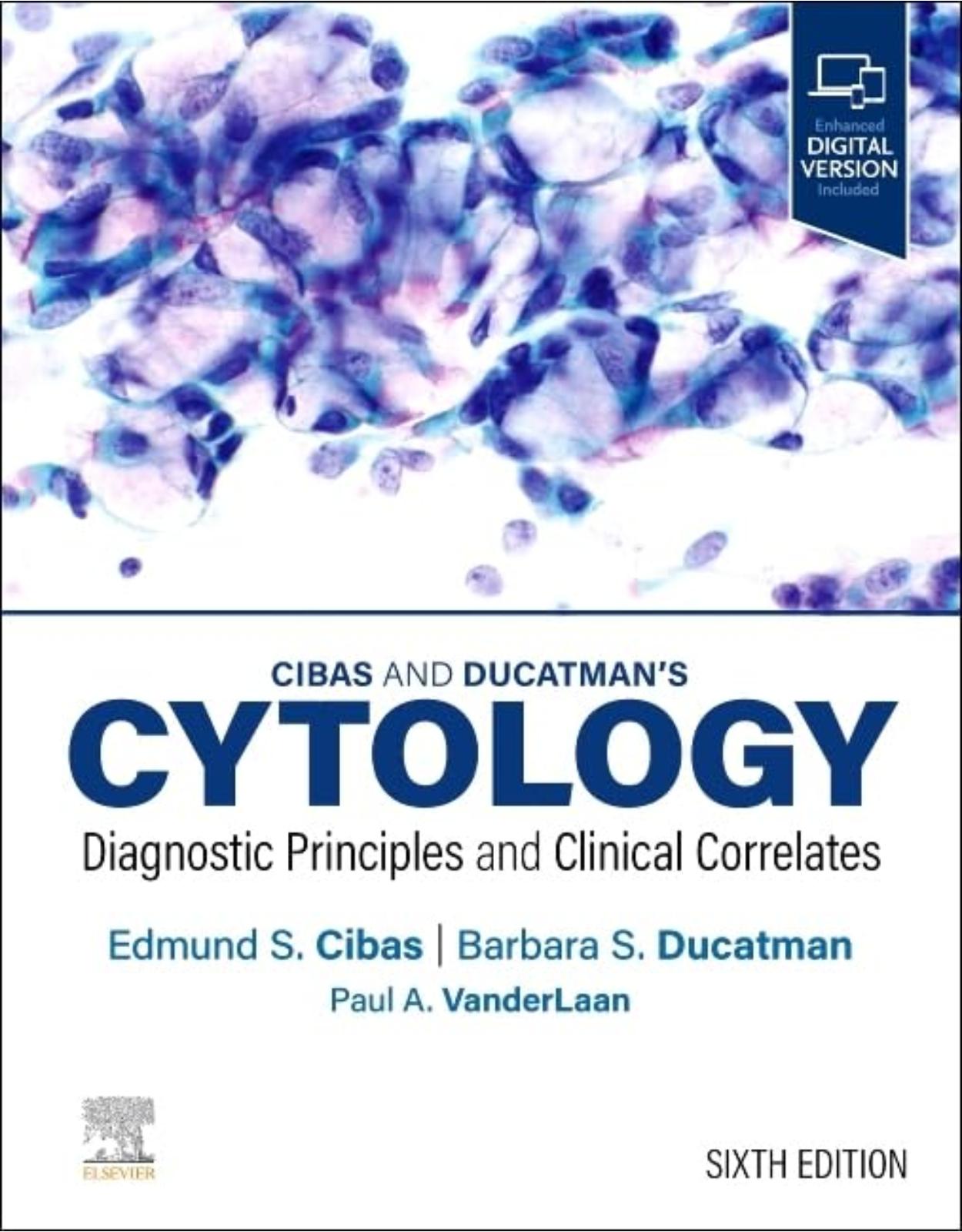
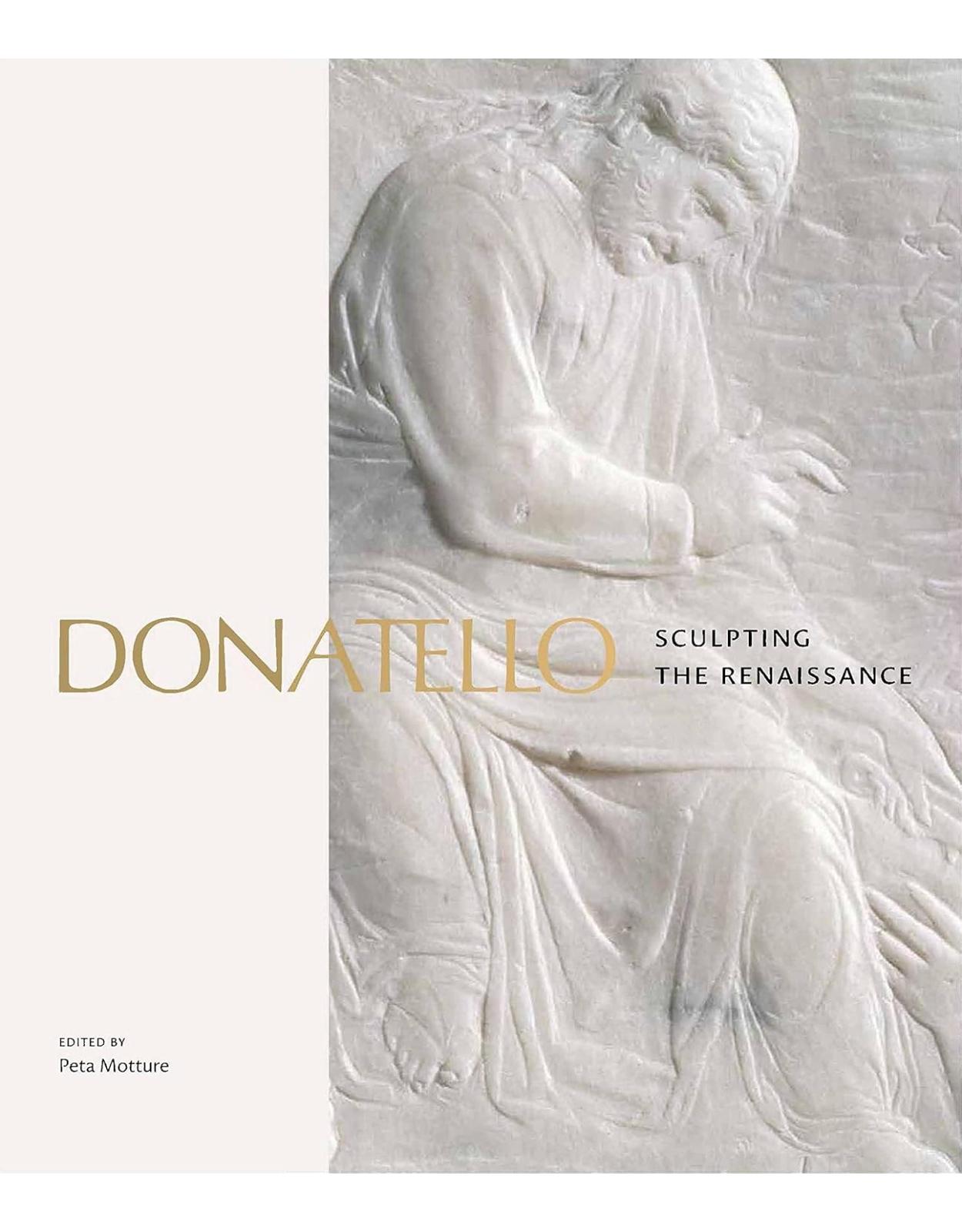
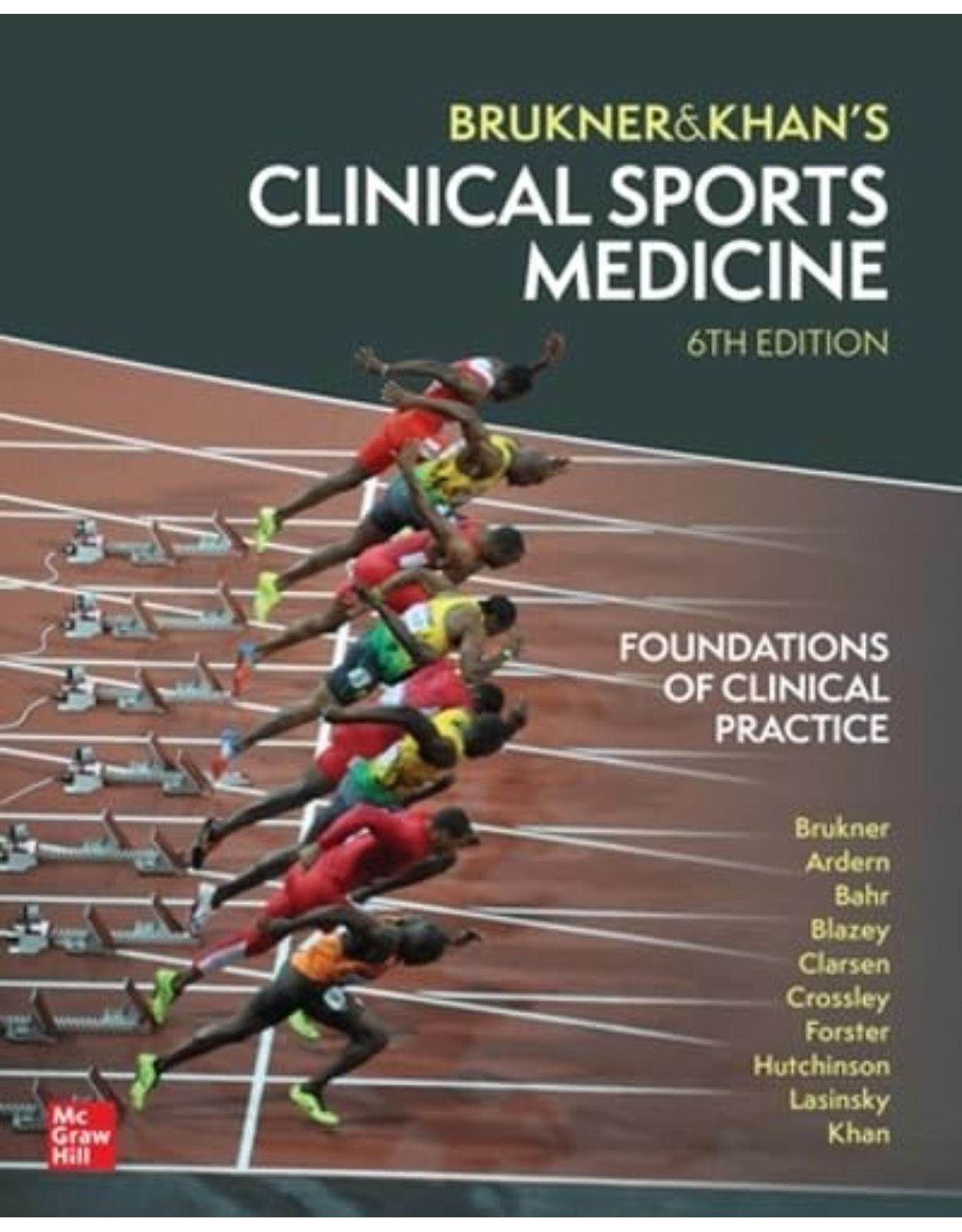
68200 lei 65000 lei
-
-
-
-
-
-
-
-
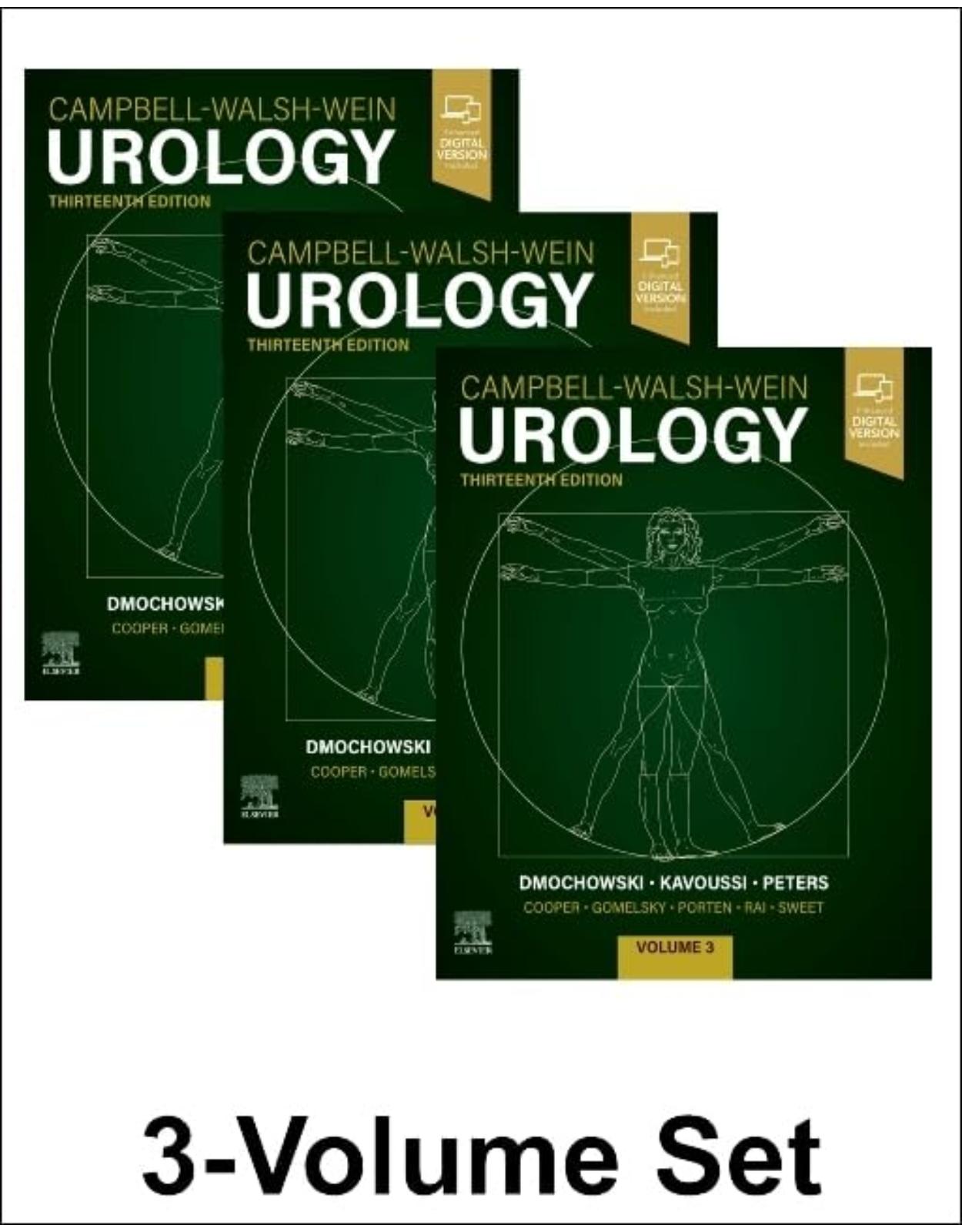
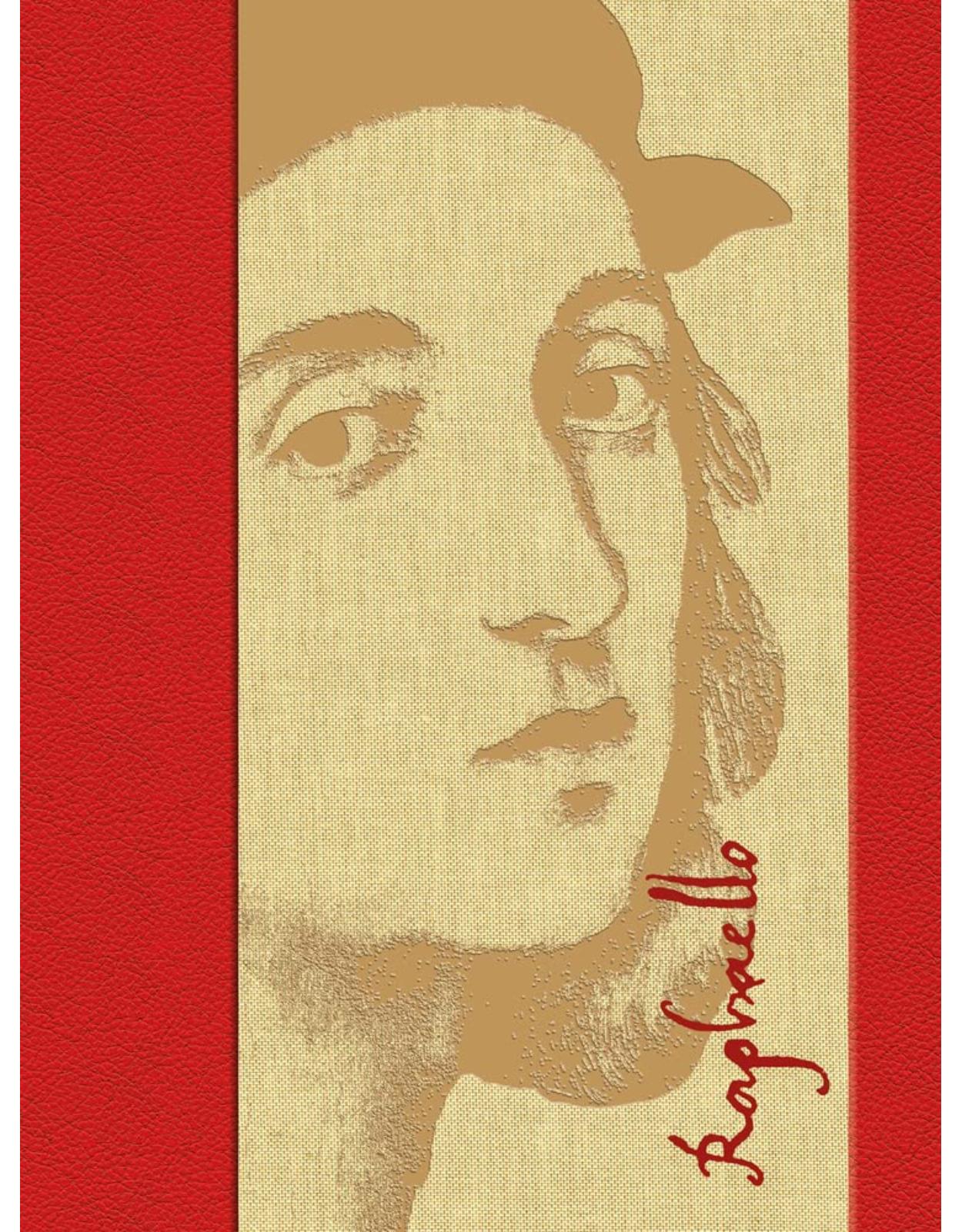
1,45400 lei 1,29500 lei
-
1,10200 lei 1,00000 lei
-
-
-
-
-
-
-
-
-
-
-
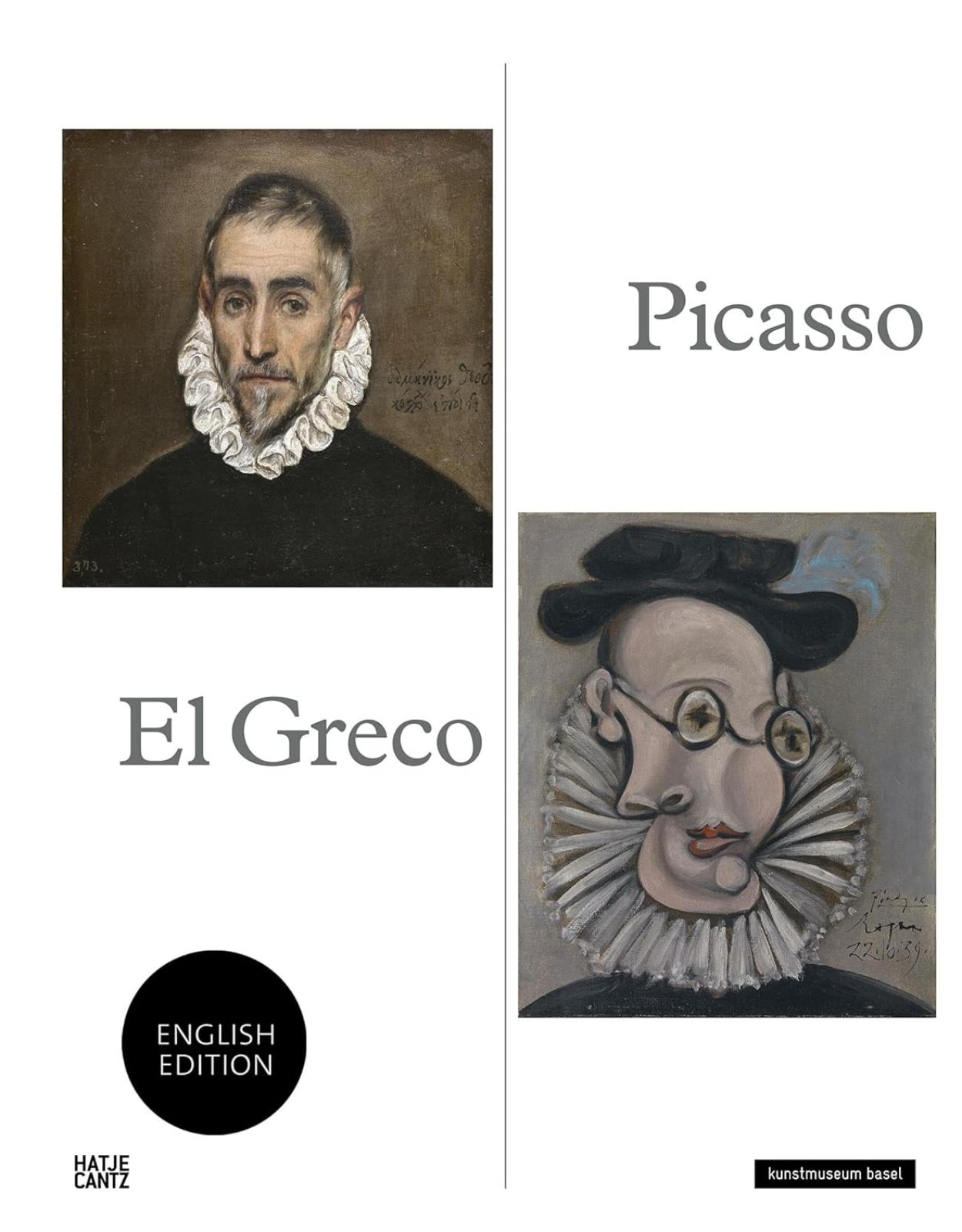
1,15500 lei 1,10000 lei
-
-
-
-
-
-
-
-
-
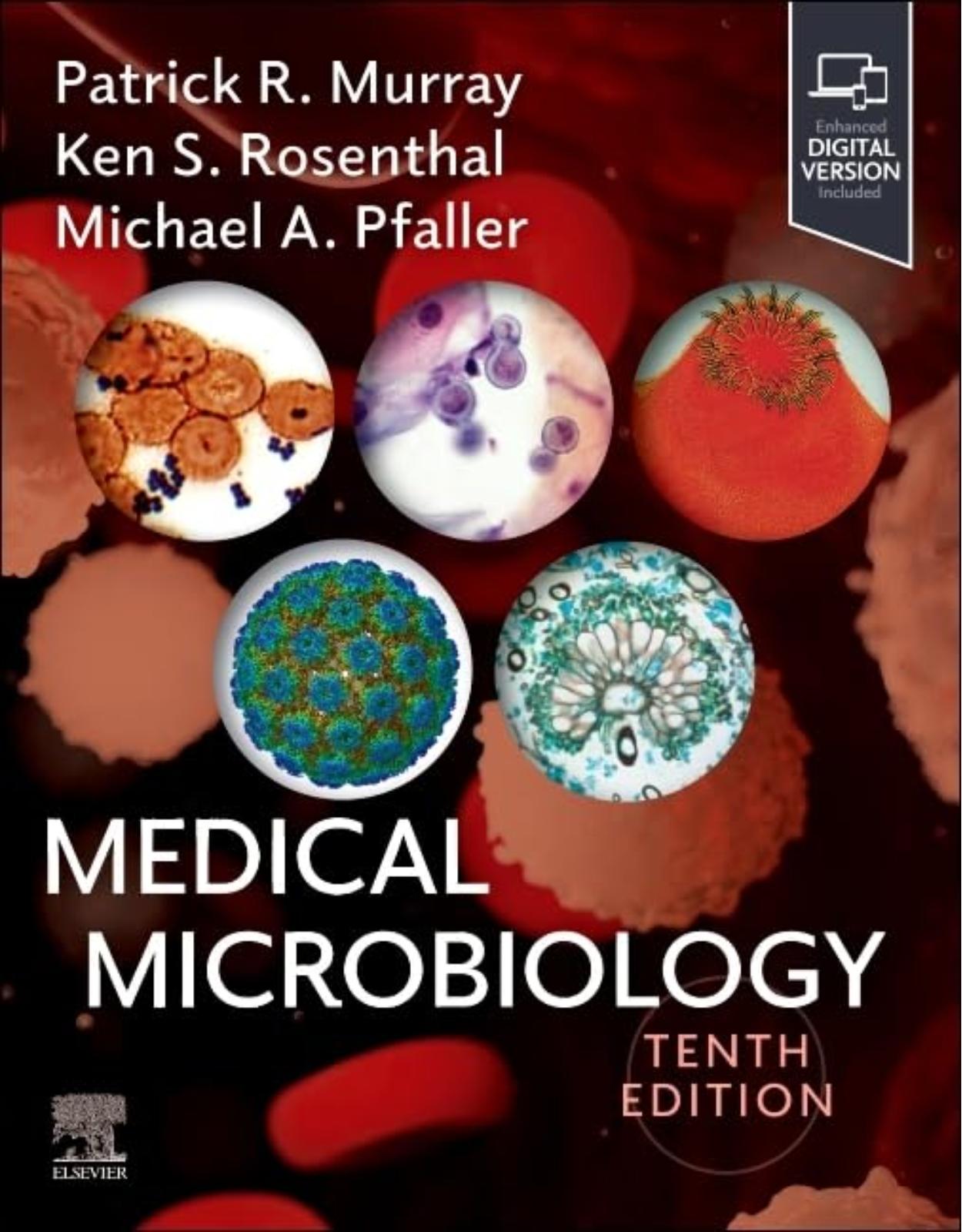
36500 lei 33000 lei
-
021.210.89.28
-

Contul meu
-

Cosul meu
Nu aveti niciun produs in cos!Transport: (0 lei)Total: 0 lei