-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
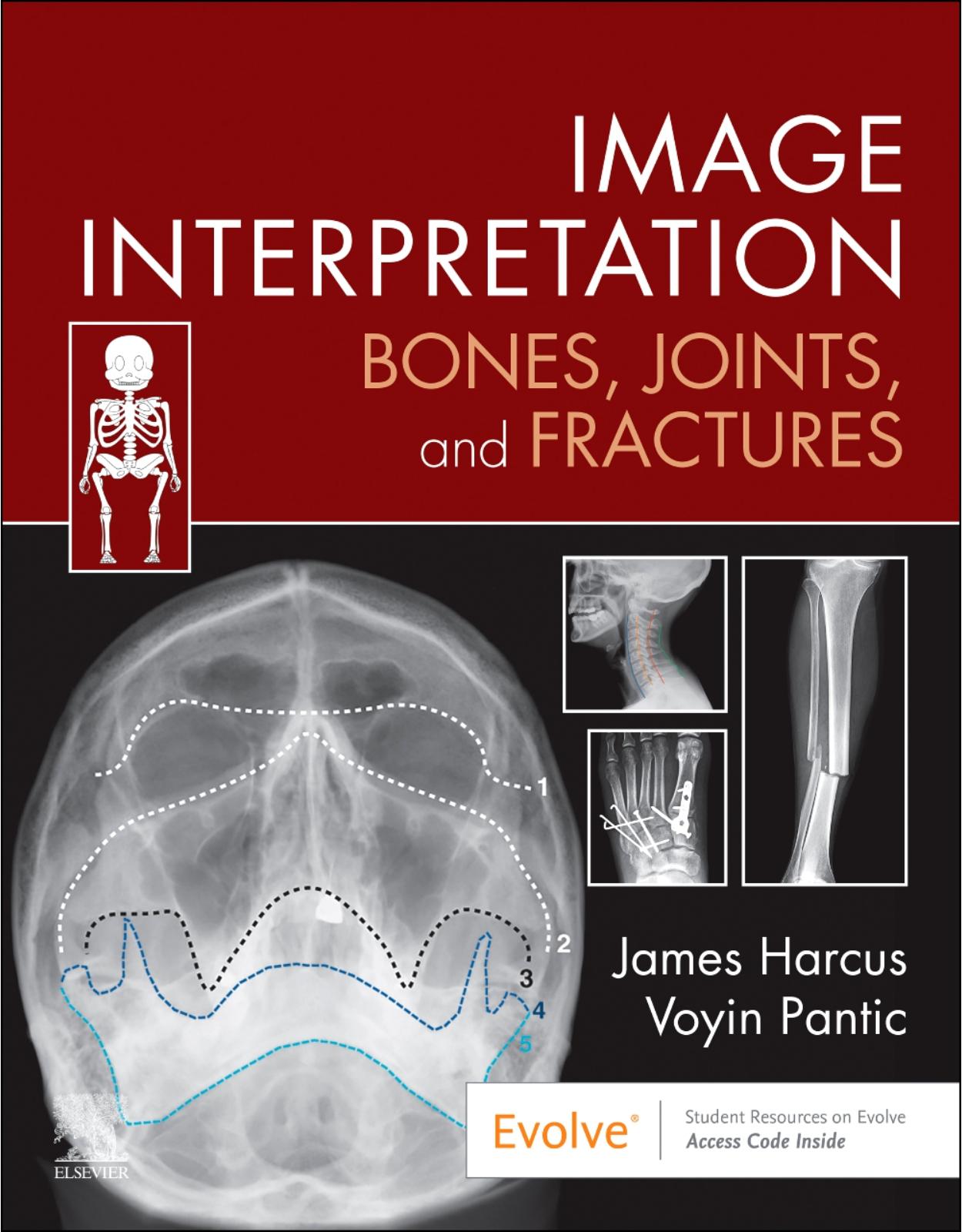
42500 lei 38100 lei
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
021.210.89.28
-

Contul meu
-

Cosul meu
Nu aveti niciun produs in cos!Transport: (0 lei)Total: 0 lei