Hunt & Marshall's Clinical Problems in Surgery, 3e
Livrare gratis la comenzi peste 500 RON. Pentru celelalte comenzi livrarea este 20 RON.
Disponibilitate: La comanda in aproximativ 4-6 saptamani
Editura: Elsevier
Limba: Engleza
Nr. pagini: 560
Coperta: Paperback
Dimensiuni: 19.05 x 2.54 x 25.4 cm
An aparitie: 06-Apr-17
Description:
Is surgery required? Is the patient effectively communicating symptoms to make the correct clinical diagnosis? Clinical Problems in Surgery, 3rd Edition supports medical students in applying clinical reasoning to problems they encounter in a clinical setup. Individual chapters are dedicated to specific regions of the body where surgeons encounter most of the problems. The content structure follows the logical step-by-step process of introducing a clinical problem; seeking history and conducting physical examination; diagnosing the patient and devising a treatment plan based on this informed diagnosis.
Table of Contents:
FIGURE 1 Iron deficiency anaemia may be A: the primary presentation of an occult carcinoma of the caecum; B: a secondary problem when carcinoma of the sigmoid presents with altered bowel habit
FIGURE 2 Forms of presentation of gastrointestinal blood loss A: melaena from a duodenal ulcer; B: occult blood loss and anaemia from a caecal carcinoma; C: acute colonic haemorrhage from diverticular disease; D: defaecatory bleeding from haemorrhoids
FIGURE 3 Forms of presentation of duodenal ulcer A: haemorrhage presenting as haematemesis and melaena; B: pyloric stenosis presenting as vomiting; C: perforation presenting as an acute abdomen. Duodenal ulcer most commonly presents as chronic epigastric pain.
The problem-oriented clinical approach
1 Collect and record the database
Take a history and examine the patient
Record the data in a systematic manner
History of the presenting complaint
Subjective data (S)
Objective data (O)
2 Constructing a problem list
3 Assessment and plan
4 Progress notes
5 Discharge summary
Medical record
Discharge summary
Student case presentations
Suggested format
What to put on visual aids such as computer presentation packages
Suggestions
Example case presentation
Format of bedside presentations
ISBAR
Chapter 1 Integument problems
1.1 Introduction
FIGURE 1.1 Focal skin lesionsA: macule; B: papule (1), nodule (2) or plaque (3); C: vesicle or pustule; D: wheal
The clinical history of a lump or ulcer
1 Onset and duration
FIGURE 1.2 Types of epithelial ulceration1. squamous cell carcinoma; 2. basal cell carcinoma; 3. venous ulcer; 4. neuropathic ulcer; 5. peptic ulcer; 6. anal fissure; 7. keratoacanthoma
2 Change and progression
3 Other symptoms
4 Multiplicity
The physical examination of a lump or ulcer
TABLE 1.1 Growth pattern of some common skin nodules
Box 1.1 Characteristics of a lump on physical examination
1 Situation and depth
2 Size
3 Shape and surroundings
4 Colour
5 Contour
6 Consistency
7 Temperature
8 Tenderness
9 Transillumination
10 Fluctuation and percussion
FIGURE 1.3 Testing fluctuationTwo watching fingers detect transmitted impulse (A) while the displacing finger applies compression (B).
11 Fixity
12 Fields
1.2 Focal skin lesions
Clearly benign lesions
FIGURE 1.4 Focal skin lesionsA: hyperkeratosis with central crusting on dorsum of hand, infective warts on index finger; B: calluses over first metatarsal head and over proximal interphalangeal joint in hammer toe
Box 1.2 Clearly benign macules and nodules in children
Pigmented lesions
Other lesions
Box 1.3 Clearly benign macules and nodules in adults
Non-pigmented lesions
Pigmented lesions
Common causes of benign skin lesions
In children
In adults
Clinical features, diagnostic and treatment plans
Children
Port-wine stain
Strawberry naevus (capillary haemangioma)
Benign mole
Intradermal, junctional and compound naevus
FIGURE 1.5 The histology of benign pigmented molesA: junctional naevus showing melanocytes at the epidermal–dermal junction; B: intradermal naevus with pigmented cells in the dermis. The histological combination of A and B is known as a compound naevus
Blue naevus
Freckles (ephelides)
Infective warts
Pyogenic granuloma
Adults
Senile freckling
Senile purpura
Callosity (callus)
Infective warts
Skin tag (benign squamous papilloma, soft fibroma)
Seborrhoeic keratosis (seborrhoeic wart)
Solar keratosis (senile keratosis, hyperkeratosis)
Sclerosing haemangioma (dermatofibroma, histiocytoma)
Senile haemangioma (Campbell-De Morgan's spots, cherry angioma)
Spider naevus
Xanthoma
Benign mole
‘Suspicious’ lesions
Causes of ‘suspicious’ skin lesions
Clinical features and diagnosis
1 Basal cell carcinoma
Box 1.4 Clinical forms of BCC
2 Squamous cell carcinoma
3 Keratoacanthoma
4 Pyogenic granuloma
5 Malignant melanoma
FIGURE 1.6 The ABCDE assessment aids in the identification of skin lesions suspicious of melanomaA: asymmetry – one half unlike the other; B: border – irregular edge; C: colour – variable pigmentation; D: diameter – usually larger than 6 mm; E: evolving – change in the lesion including increasing elevation
6 Kaposi sarcoma
Treatment plans
1 Basal cell carcinoma
2 Squamous cell carcinoma
3 Keratoacanthoma
TABLE 1.2 Malignancies and their mimics
4 Pyogenic granulomas
5 Melanoma
Box 1.5 Suspicious pigmented lesions
FIGURE 1.7 Prognosis in malignant melanoma is measured in two ways: depth of invasion (Clark's levels I–V) or simple measurement of tumour depth in millimetresComparison of the two methods is shown. Level I: an in situ lesion above the basement membrane of the basal layer of the epidermis, less than 0.75 mm in depth. Level II: the lesion is invading into the papillary dermis, equivalent to a depth 0.75–1.5 mm. Level III: the lesion fills the papillary dermis down to its junction with the reticular dermis, a depth of 1.5–2.25 mm. Level IV: the lesion extends into the reticular dermis, a depth of 2.25–3.0 mm. Level V: well into the subcutaneous tissue, a depth greater than 3.0 mm
TABLE 1.3 Tumour depth in melanoma influences management and prognosis
6 Kaposi sarcoma
7 Other malignant or infective skin lesions
Pigmented skin lesions
TABLE 1.4 Types of benign pigmented moles
Diagnostic and therapeutic plans
Box 1.6 Pigmented skin lesions – indications for excision
1.3 Subcutaneous lumps
Common causes
Clinical features and treatment plan
1 Lipoma
FIGURE 1.8 Lipoma and sebaceous cystA: the surface contour of a lipoma is classically lobulated; B: when a lipoma is pressed, it tends to slip from beneath the finger; C: these features are not seen in sebaceous cyst, which is fixed to the skin, has a spherical shape and a smooth contour
2 ‘Sebaceous’ cyst
FIGURE 1.9 Excision of a lipomaA–C: most lipomas can be shelled out after infiltration with a local anaesthetic and an incision directly over the lesion
FIGURE 1.10 Excision of a sebaceous cystInfiltration of local anaesthetic. A: bisection through the punctum and avulsion of each half using an artery forcep; B: formal excision using an elliptical incision. The cyst is freed from the subcutaneous tissue by blunt dissection.
3 Ganglion
FIGURE 1.11 Ganglion on the dorsum of the wrist joint is made more prominent by hyperflexion of the joint
4 Bursa
5 ‘Dermoid’ cysts
6 Neurofibromas
1.4 Cutaneous and subcutaneous infections
Pathology
Clinical features
Diagnosis and treatment plans
General principles
1 The primary site of infection
Box 1.7 The general principles of the treatment of surgical infection
FIGURE 1.12 Incision and drainage of subcutaneous infectionA: the central area of the abscess is infiltrated with local anaesthetic; B: the abscess is incised to allow free drainage; C: an appropriate dressing is used to allow the cavity to heal by secondary intention
2 The infectious agent
3 The susceptible host and measures to strengthen host resistance
Specific infections of skin and subcutaneous tissues
Common types
Clinical features and treatment plan
1 Infected epidermoid (sebaceous) cysts
2 Folliculitis, furuncle, carbuncle, hydradenitis
3 Erysipelas, cellulitis, impetigo
4 Necrotising soft tissue infections
5 Specific sites
1.5 Lymph node swellings
FIGURE 1.13 The Karydakis operation for chronic pilonidal sinusA: one side of the incision is placed further from the midline; B: the sinus and surrounding fibrous tissue is excised down to the fascia over the sacrum, creating a flap on one side; C: closure brings the flap away from the midline, avoiding a central unstable scar and thus reducing the chance of recurrence
FIGURE 1.14 Lymph nodes in the neck1: submental nodes drain the lip; 2: submandibular nodes drain the anterior two-thirds of the tongue, floor of mouth, gums and buccal mucosa; 3: upper jugular nodes of the deep cervical chain drain the oral cavity, nasopharynx, tonsil, base of the tongue, pharynx and larynx; middle nodes drain the thyroid, pyriform sinus and larynx; 4: supraclavicular nodes from the arm and mediastinum; 5: posterior triangle nodes drain the nasopharynx; 6: mastoid nodes drain the nasopharynx and parotid; 7: suboccipital nodes drain the posterior scalp; 8: pre-auricular nodes drain the scalp, ear and parotid; A: Stohr's node; B: the tonsillar node; C: Virchow's node; D: the Delphic node. Intralymphatic deposits of melanoma are visible on the chest wall together with a left axillary mass due to lymphadenopathy
FIGURE 1.15 Lymph nodes in the axillaA: the axilla can be exposed by abducting and/or extending the arm; B: the axilla can be considered a pyramidal space with the lymph node groups arranged as numbered below.1. subscapular nodes; 2. pectoral nodes drain lymph from the breast; 3. central nodes drain lymph from the breast and back; 4. apical nodes drain the other axillary node groups and are continuous with the supraclavicular nodes; 5. lateral nodes
FIGURE 1.16 Lymph nodes in the groin1. vertical group of superficial inguinal nodes drain the lower limb; 2. horizontal group of superficial inguinal nodes. The lateral group drain back below the iliac crest and the medial group drain the anterior abdominal wall, below the umbilicus, the perineum and external genitalia and the lower half of the anal canal; 3. deep inguinal nodes including the node of Cloquet (4) collect deep and superficial lymph fluid
Common causes
Localised lymph node swellings
Generalised lymph node swellings
Clinical assessment
Localised lymph node swellings
Generalised lymph node swellings
Diagnostic and treatment plans
Chapter 2 ENT, Head and neck problems
2.1 Introduction
History
Examination of the head and neck
Ear
Nose
Nose and sinuses
TABLE 2.1 Symptoms of ear, nose and throat conditions
TABLE 2.2 Referred or non-otologic otalgia
Throat
Mouth
Oropharynx
Hypopharynx
Nasopharynx
Head and neck lumps
FIGURE 2.1 Division of lymph node groups levels I–VI (VII)
TABLE 2.3 Thyroid examination – performed if thyroid disease is detected or suspected
TABLE 2.4 Screening examination of the cranial nerves
FIGURE 2.2a and b Voroscope
FIGURE 2.3 Nasolaryngoscope
Regional and developmental anatomy
2.2 Ear
TABLE 2.5 Outer ear, middle ear and inner ear components
FIGURE 2.4 Anatomy of the ear
Role of the ear
Nearby blood vessels
External ear
Wax and otitis externa
Management
Middle ear
Otitis media
FIGURE 2.5a Extracranial complications of otitis media
FIGURE 2.5b Intracranial complications of otitis media
Inner ear
Hearing loss
TABLE 2.6 Causes of hearing loss
Vertigo
Tinnitus
FIGURE 2.6 Tuning fork tests
FIGURE 2.7 Audiograms
FIGURE 2.8 Otologic causes for dizziness
TABLE 2.7 Causes of tinnitus
2.3 Facial weakness
Trauma
2.4 Nose and sinuses
Anatomy/physiology
FIGURE 2.9 Structure of the lateral nasal wall
Blood supply
Nerve supply
Olfactory nerve – cranial nerve I
FIGURE 2.10 Paranasal sinuses
Paranasal sinuses
Epistaxis
Nasal obstruction
Sinusitis, nasal polyps, allergy
Investigations
Treatment
2.5 Throat
Tonsils and adenoids
FIGURE 2.11 Laryngeal framework
TABLE 2.8 Related spaces and anatomy
Anatomy
Microbiology/pathology
Infectious mononucleosis
History and examination
TABLE 2.9 Organisms found in the tonsil
Diagnosis
Medical treatment
Surgical treatment
FIGURE 2.12 Bacterial tonsillitis
FIGURE 2.13 Infectious mononucleosis
2.6 Airway emergencies and tracheostomy
FIGURE 2.14 Quinsy
Tube types
FIGURE 2.15 Tracheostomy tubes
Complications
Avoiding complications
2.7 Snoring and obstructive apnoea
Treatment
2.8 Voice, dysphonia, hoarse voice
Anatomy
Nerve supply
Dysphonia
FIGURE 2.16 The larynx
TABLE 2.10 The anatomy of the larynx
TABLE 2.11 Organic and non-organic causes of dysphonia
2.9 Dysphagia
2.10 Congenital anomalies
Thyroglossal cysts
Branchial cysts
FIGURE 2.17 Congenital anomaliesa. Thyroglossal duct cyst
b. Type II Branchial cleft cyst
Vascular malformations
Nasolabial cyst, dermoids, cleft lip and cleft palate
2.11 Foreign bodies
Ear
History
Examination
Investigation
Treatment
Nose
History
Examination
Investigation
Treatment
Oropharyngeal/oesophageal
History
Examination
Investigation
Treatment
Upper airway
History
Examination
Investigation
Treatment
2.12 Head and neck cancer
2.13 Larynx
TABLE 2.12 TNM
Larynx
2.14 Parotid and salivary glands
TABLE 2.13 Staging for lip and oral cancer
TABLE 2.14 Staging for oropharyngeal carcinoma
TABLE 2.15 Staging for hypopharyngeal carcinoma
TABLE 2.16 Staging for nasopharyngeal carcinoma
TABLE 2.17 Staging for supraglottic carcinoma
FIGURE 2.18 Carcinoma of tonsil
TABLE 2.18 Staging for glottic carcinoma
TABLE 2.19 Staging for subglottic carcinoma
TABLE 2.20 Staging for salivary gland carcinoma
Investigations
2.15 Thyroid/parathyroid
Goitre
Common causes
Clinical features
History
TABLE 2.21 Physical examination of the thyroid
Common causes – specific clinical features
I General enlargements
1 Multinodular goitre
2 Graves' disease
3 Hashimoto's thyroiditis
4 Anaplastic carcinoma
II Single nodule
Benign lesion
FIGURE 2.19 Goitre – single noduleA: dominant nodule in a multinodular goitre; B: benign adenoma; C: celloid nodule within a haemorrhagic cyst; D: carcinoma (papillary) with nodes
Carcinoma
TABLE 2.22 Thyroid carcinoma classification and staging
TABLE 2.23 Staging papillary or follicular carcinoma
TABLE 2.24 Staging undifferentiated – anaplastic carcinoma
TABLE 2.25 Thyroid carcinoma outcome statistics
TABLE 2.26 The Mayo Clinic carcinoma classification system
TABLE 2.27 The Lahey Clinic's AMES classification
Diagnosis
Thyroid function tests
Thyroid imaging
Aspiration cytology
Other biochemical tests
Treatment plan
I General enlargement
Generalised longstanding gland enlargement (multinodular goitre)
Graves' disease
Hashimoto's thyroiditis
Anaplastic invasive cancer
II Solitary thyroid nodules
2.16 Mouth ulcers and lesions
Common causes
Clinical features and treatment
Benign disease
Benign ‘dental’ ulcer
Herpes labialis (‘cold sore’)
Benign fissures and crusting of mucous membrane
Prosthetic ulcers and epulides
Pyogenic granuloma
Lichen planus
Candidiasis
Mucous retention cyst
Neutropenia
Pigmented and vascular lesions
Premalignant lesions
2.17 Approach to a head and neck lump
2.18 Neck pain
Clinical features, diagnostic and treatment plans
Cervical spondylosis and cervical disc degeneration
Whiplash
Cervical rib
Referred pain
Other causes
2.19 Cranial nerve evaluation
First (olfactory) cranial nerve
Second (optic) cranial nerve
Third, fourth and sixth cranial nerves
Fifth cranial nerve (trigeminal)
Seventh (facial) cranial nerve
Eighth cranial nerve
Ninth and tenth cranial nerves (glossopharyngeal and vagus)
Eleventh cranial nerve (accessory)
Twelfth cranial nerve (hypoglossal)
Chapter 3 Breast problems
3.1 Introduction
History
Physical examination
Box 3.1 Causes of unilateral enlargement of the breast or breast asymmetry
FIGURE 3.1 Asymmetrical breast development
FIGURE 3.2 Accessory nipple
FIGURE 3.3 Accessory breast tissue in the axilla
FIGURE 3.4 Upper outer breast distortion
FIGURE 3.5 Skin tethering due to cancer only demonstrable when the patient raises her arms
FIGURE 3.6 Breast examination
FIGURE 3.7 Scheme for recording the characteristics of breast lesions
Diagnostic tests
Imaging techniques: mammography, ultrasound
Cytology and histology
3.2 Breast pain
Common causes
Clinical features and diagnosis
FIGURE 3.8 Mammographic and sonographic images of the breastMammographic and sonographic images of the breast often demonstrate the features of benign and malignant breast lesions. (a) Breast cancer typically appears on a mammogram as a focal density with spiculate edges. (b) Microcalcification can be associated with benign and malignant breast pathology and is graded according to its morphology. Typically malignant calcification is variable in size and shape and may cast the branching pattern of the milk ducts. (c) Simple cysts may show as a discrete density on mammography, but ultrasound best demonstrates the smooth cyst wall and anechoic cyst fluid. (d) Fibroadenomas may also appear as a discrete density on mammography and on ultrasound. A benign solid lesion should have more breadth than height.
Treatment plan
3.3 Breast lump
Causes
History and physical examination
1 Carcinoma
FIGURE 3.9 Locally advanced breast cancer
Box 3.2 Breast cancer staging
Primary tumour (T)
Regional lymph node involvement (N)
Metastatic involvement (M)
2 Involutional change with stromal hyperplasia
3 Fibrocystic change (breast cyst)
4 Fibroadenoma
5 Mammary duct ectasia
6 Less common causes
Diagnostic plans
1 Fine needle aspiration cytology
2 Mammography
Treatment plan
1 Clinical staging
2 Curative surgical treatment for early disease
4 Stage IV disease and advanced local disease
3.4 Nipple discharge
TABLE 3.1 Differences between Paget's disease and eczema of the nipple
Common causes
Diagnostic plans
Discharge from many duct orifices (often bilateral)
FIGURE 3.10 Paget's disease of the nipple
FIGURE 3.11 Eczema affecting the areola
Unilateral bloody discharge from a single duct
FIGURE 3.12 Multiduct discharge in duct ectasia
FIGURE 3.13 Single duct discharge suggestive of a papilloma
Mammary duct fistula
FIGURE 3.14 Nipple discharge A spot of fluid is seen to appear from a single duct with pressure on the related breast segment.
Diagnostic plan
Treatment plan
FIGURE 3.15 MicrodochectomyA: identification of affected duct by local pressure and insertion of lacrimal probe; B: excision of a segment containing the duct and papilloma through a circumareolar incision
3.5 Gynaecomastia
Common causes
Clinical features
1 Puberty and old age
2 Systemic disease
3 Carcinoma of the lung and other tumours
4 Drug-induced gynaecomastia
Box 3.3 Common drugs associated with gynaecomastia
Diagnostic plan
Treatment plan
Chapter 4 Chest and chest wall problems
4.1 Introduction
Box 4.1 Assessment of exercise tolerance
History
TABLE 4.1 New York Heart Association classification of angina
Physical examination
General inspection
Examination of the periphery
TABLE 4.2 Grades of finger clubbing
Examination of the pulse
Examination of the head and neck
Jugular venous pressure and pulse
TABLE 4.3 Venous and arterial pulses and pressures in the neck
Examination of the heart
TABLE 4.4 Clinical manifestations of heart failure
Examination of the chest and lungs
4.2 Acute chest pain
Causes
Clinical features
1 Angina pectoris, myocardial infarction and oesophageal spasm
2 Pneumothorax
3 Pleurisy and pneumonia
4 Pulmonary embolus and infarction
5 Musculoskeletal disorders
6 Less common causes
Diagnostic plans
Chest x-ray
FIGURE 4.1 Chest x-ray showing an apical pneumothorax
Electrocardiogram
FIGURE 4.2 Chest x-ray showing a right-sided tension pneumothorax
FIGURE 4.3 Chest x-ray showing a pericardial effusion
Serum enzymes
Plasma D-dimers
Arterial blood gases
Ventilation/perfusion (V/Q) scanning
Echocardiography
Computed tomography pulmonary angiography (CTPA)
FIGURE 4.4 Computed tomography pulmonary angiogram (CTPA) showing a large pulmonary embolus (arrowed)
Lower limb venous Doppler
Gastrografin swallow
Treatment plans
1 Myocardial infarction (and oesophageal spasm)
2 Pneumothorax, tension pneumothorax, cardiac tamponade
3 Pleurisy and pneumonia
4 Pulmonary embolus
5 Musculoskeletal pain
6 Other causes
4.3 Pleural effusion
Common causes
I Transudate
II Exudate
Clinical features
Investigations
FIGURE 4.5 Chest x-ray showing a large left-sided pleural effusion
Treatment plans
4.4 Chronic cough and haemoptysis
Causes
Clinical features
1 Smokers' lungs
2 Carcinoma of the lung
TABLE 4.5 Pathological types of lung cancer
3 Postviral bronchitis
4 Foreign body
TABLE 4.6 Causes of coin lesion in the lung on chest x-ray
5 Tuberculosis
Diagnostic plans
Imaging
Endoscopic studies
FIGURE 4.6 Chest x-ray showing a lung cancer
FIGURE 4.7 CT scans showing a lung cancer
Box 4.2 TNM staging of lung cancer
Primary tumour (T)
Regional lymph node involvement (N)
Metastatic involvement (M)
Box 4.3 Stage groupings for lung cancer
Box 4.4 Five-year survival for the various stages of lung cancer
Treatment plan
1 Smokers' lungs
2 Carcinoma of the lung
3 Postviral bronchitis
4 Foreign body
5 Tuberculosis
6 Less common causes
4.5 Chest wall problems
Common causes
Clinical presentation and management plans
1 Congenital deformities of the thoracic cage
2 Soft tissue swellings
3 Bony swellings
4 Costochondral swellings
5 Infections
Chapter 5 Back and related limb neurological problems
5.1 Introduction: the back and spine
History
Examination
FIGURE 5.1 Straight leg raising test for nerve root compression
Neurological system
History
Examination
Motor nerve function
TABLE 5.1 The nerve and spinal roots that innervate the major muscle groups of the upper limb
Sensory nerve function
TABLE 5.2 The nerve and spinal roots that innervate the major muscle groups of the lower limb
Reflex function
FIGURE 5.2 Sensory dermatomes of the body
TABLE 5.3 The spinal segments involved in the common stretch reflexes
Gait
5.2 Back pain
Causes
Special tests in the assessment of spinal pain
Chronic lumbar ligamentous strain
Degenerative disc disease, spondylosis and osteoarthritis
FIGURE 5.3 Pathological sequence in degenerative back diseaseA: normal lumbar vertebrae and disc; B: herniation of the nucleus pulposus; C: disc space degeneration and flattening with early osteoarthritis of the facet joint; D: advanced lumbar degenerative spine disease with facet joint osteophyte formation and compression of the nerve root. Forward slip and arthritis may also lead to narrowing of the spinal canal.
Spondylolisthesis
Osteoporosis
Secondary carcinoma of the vertebral body
FIGURE 5.4 Vertebral collapseA: infection – the vertebral body appears intact because the infection usually lies adjacent to the disc; B: metastatic disease of vertebra leads to collapse with apparent preservation of the adjacent disc. Both conditions lead to kyphosis.
Spinal infection
Referred pain
Less common causes
Diagnostic plan
Treatment plan
5.3 Limb weakness and numbness – peripheral neuropathies
Clinical assessment of specific nerve palsies
Upper limb nerve palsies
Lower limb nerve palsies
Median nerve
Common causes
FIGURE 5.5 Median nerve lesionsThe long flexor of the thumb is tested by flexion of the distal interphalangeal joint against resistance.
Ulnar nerve
Common causes
FIGURE 5.6 Ulnar nerve lesionThe little finger is abducted away from the other fingers against resistance.
FIGURE 5.7 Ulnar nerve lesion – Froment's signOn the side that the adductor pollicis is weak, the patient can only hold the card by flexing the terminal joint of the thumb.
FIGURE 5.8 Causes of finger deformities and clawingA: normal finger; B: claw hand (ulnar nerve or T1 lesion); C: Volkmann's ischaemic contracture; D: intrinsic plus hand; E: Dupuytren's contracture
Radial nerve and posterior interosseous nerve
Common causes
Axillary (circumflex) nerve
Common cause
Brachial plexus
Common causes
Spinal nerve root lesions (cervical)
Lower limb: common peroneal nerve
Common causes
Posterior tibial nerve
Common causes
Sciatic nerve
Common causes
Femoral nerve
Common causes
Lumbo-sacral plexus and roots
Common causes
5.4 Limb weakness – other causes
Weakness with wasting
Wasting without sensory loss
Causes of wasting with normal sensation
Clinical features
1 Posttraumatic disuse
2 Motor neurone disease
3 Poliomyelitis
4 Purely motor peripheral neuropathy
5 Myopathy
Weakness without wasting
Central nervous system lesions – hemiplegia
Common causes
Clinical features
Deformity and posture
Muscle weakness without wasting
Hypertonicity
FIGURE 5.9 Typical features of hemiplegia
Diagnostic plan
Vascular stroke
Neurotrauma
FIGURE 5.10 Extracranial carotid bifurcation diseaseA: normal carotid arteries; B: severe stenotic plaque at internal carotid artery with emboli; C: post carotid endarterectomy and standard repair with patch at endarterectomised site
FIGURE 5.11 Carotid fibromuscular dysplasia
Treatment plan
Spinal cord lesions – paraplegia or quadriplegia
FIGURE 5.12 Carotid stentingA: angiographic appearance of severe internal carotid artery stenosis; B: carotid stent placed across the stenosis
Common causes
With compression
Without compression
History, examination and clinical assessment
Hemisection of the spinal cord (Brown-Séquard syndrome)
Diagnostic and treatment plans
Chapter 6 Limb problems
6.1 Introduction
Arterial circulation
History
Examination
Inspection
Palpation
FIGURE 6.1 Temperature change detected by applying the thin skin of the dorsal surface of the fingers to the lesions
FIGURE 6.2a The midinguinal pointA: lies halfway between the anterior superior iliac spine (1) and symphysis pubis (2) the deep inguinal ring; B: lies above the midpoint of the inguinal ligament, which attaches to the pubic tubercle (3); C: common femoral artery; D: common femoral vein; E: saphenous opening; F: great saphenous vein
FIGURE 6.2b The anatomy of the arterial system
Auscultation
Venous circulation
History
Examination
Inspection
Palpation
Neurological system
History
Examination
Motor nerve function
Sensory nerve function
Reflex function
Gait
Musculoskeletal locomotor system
History
Examination
Inspection
Palpation
Movement
6.2 Bony lumps
FIGURE 6.3 Apparent and true shorteningA: adduction deformity of the left leg. The legs are kept in line by pelvic tilt and the leg is apparently short (measured from umbilicus); B: when the pelvis is set square and the legs are matched for position the difference in length disappears; C: true shortening of the left leg (measured from ASIS) at the hip or femoral neck. Measured with the pelvis square and the legs matched for position.
FIGURE 6.4 Typical sites of long bone tumoursA: an expanding swelling at the end of the bone is likely to be a giant cell tumour; B: a swelling to one side at the epiphysis is likely to be an exostosis; C: a swelling in the region of the metaphysis may be osteosarcoma, chronic osteomyelitis (Brodie's abscess) or a simple or aneurysmal bone cyst; D: a swelling in the middle of a long bone may be an eosinophilic granuloma, Ewing's sarcoma or callus formation
TABLE 6.1 Common causes of localised swelling of bone
Causes
History, physical examination and radiology
1 Callus formation
2 Acute osteomyelitis
3 Osteosarcoma
FIGURE 6.5 Bone infection commonly starts in the metaphysis below the epiphyseal plateA: the plate acts as a barrier to spread into the joint;B: spread through the cortex forms a subperiosteal abscess;C: stripping of the periosteum interrupts the blood supply to the cortex, which forms a sequestrum; the sequestrum forms a nidus for chronic ostemyelitis
4 Giant cell tumour of bone
5 Fibrosarcoma
6 Chondrosarcoma
7 Metastatic carcinoma
8 Less common causes
Diagnostic and treatment plans
FIGURE 6.6 Radiological features of common bone tumoursA: ecchondroma may be painful or may fracture; B: enchondromas are often multiple and may also fracture; C: osteoid osteoma is associated with increasing bone pain; D: osteosarcoma produces destruction of the cortex, elevation of the periosteum (Codman's triangle) and sunray appearance; E: osteoclastoma is a radiolucent lesion expaling the cortex and may extend to the articular surface
6.3 Musculotendinous lumps
FIGURE 6.7 A lump located within a muscleA: lumps superficial to muscle remain easy to feel when the muscle contracts; B: lumps within muscle become obscured or impalpable when the muscle contracts
Muscle swellings
Causes
Tendinous swellings
Cause
Clinical features, diagnostic and treatment plans of musculotendinous lumps
Muscle swellings
1 Muscle rupture
FIGURE 6.8 Ruptured long head of biceps brachii
2 Intramuscular haematoma
3 Muscle hernia
4 Benign or malignant intramuscular neoplasms
5 Less common causes
Tendinous swellings
Stenosing tenosynovitis
6.4 Painful shoulder
FIGURE 6.9 Surface landmarks of the shoulder1: clavicle; 2: coracoid process; 3: bicipital groove; 4: greater tuberosity; 5: acromion; 6: subacromial bursa
Causes
History and physical examination
1 Rotator cuff lesions
FIGURE 6.10 Anatomical basis of rotator cuff disordersA: 1: inflamed subacromial bursa; 2: degeneration and calcification of the supraspinatus tendon; B: the painful arc of shoulder movement through 60° and 120° of shoulder abduction
2 ‘Frozen’ shoulder
3 Bicipital tendinitis and rupture
4 Osteoarthritis of the acromioclavicular joint
5 Referred pain
6 Less common causes
Diagnostic plan
Treatment plan
6.5 Pain in the upper limbs
Common causes
Clinical features and diagnosis
1 Carpal tunnel syndrome
2 Tennis elbow
FIGURE 6.11 Tennis elbowA: the site of tenderness is over the extensor tendons just anterior to the lateral epicondyle
3 De Quervain's tenosynovitis
4 Repetitive strain injury
FIGURE 6.12 De Quervain's tenosynovitisThickening in the sheath of abductor pollicis longus and extensor pollicis brevis (A) where they cross the styloid process of the radius (B)
Treatment plan
6.6 Subcutaneous hand lumps
Causes
Clinical features and diagnostic plan
1 Ganglion
FIGURE 6.13 Dorsal wrist ganglionA: sectional view; B: surface view of a ganglion presenting between slips of the extensor digitorum longus
2 Synovioma of tendon sheath (benign giant cell tumour, xanthoma)
FIGURE 6.14 Ganglion1: sesamoid ganglia on the lateral palmar aspect of the metacarpophalangeal joints arising from the fibrous flexor tendon sheath; 2: sesamoid bones lie medially in relation to the volar aspect of the thumb
3 Dupuytren's disease
4 Traumatically induced lesions
5 Nodules associated with joint disease
6 Less common causes
Treatment plan: general
6.7 Hand deformities
FIGURE 6.15 The stronger power gripA: precision grip depends on the pinching movement; B: power grip requires wrist, elbow and shoulder as well as hand power
FIGURE 6.16 Skin incisionsSkin incisions are best placed in flexure skin creases, along lines of cleavage or along the lateral margins of the fingers in areas of relative skin immobility. Zig-zag oblique incisions between joint flexure lines ensure that the incision does not cross the crease line at right angles.
Common causes
FIGURE 6.17 Correct hand splinteringA: the position of function. The wrist is extended and the fingers progressively flexed; B: the position of rest of the hand and fingers. The wrist is in neutral; C: splintage position. Wrist extended, flexed metacarpophalangeal joints and relatively straight fingers (Z-position).
History and physical examination
1 Congenital contractures
2 Wound contractures
3 Dupuytren's contracture
FIGURE 6.18 Dupuytren's contracture
4 Ischaemic muscle contracture (Volkmann's)
FIGURE 6.19 Volkmann's contractureA: moderate flexion of the wrist with gross flexion of the interphalangeal joints; the metacarpophalangeal joints are in the neutral position or slightly extended; B: the thumb is partly spared in this case
5 Tendon disorders
FIGURE 6.20 The ‘intrinsic plus’ handThe intrinsic plus hand results from fibrous contracture or hypertonicity of the small muscles of the hand. Flexion of the metacarpophalangeal joints, interphalangeal joint extension and adduction of the thumb.
FIGURE 6.21 Trigger finger from stenosing tenosynovitis of the flexor tendonThe finger becomes locked in flexion. Forced extension leads to a sudden click and release.
FIGURE 6.22 Mallet fingerA: extensor tendon avulsion; B: avulsion of bone fragment, tendon intact
FIGURE 6.23 Boutonnière deformityA: normal tendon B: ruptured central slip; C: established deformity
FIGURE 6.24 Swan neck deformity
6 Deformities due to arthritis
7 Deformities due to neurological lesions
FIGURE 6.25 Rheumatoid hand1: ‘swan neck’ finger deformity; 2: mallet finger; 3: flexion contracture of M-P joint; 4: Z-thumb deformity; 5: muscle wasting; 6: synovial thickening; 7: thickening of the dorsal ligaments of the proximal interphalangeal joints; 8: ulnar deviation of fingers
FIGURE 6.26 Claw hand due to ulnar nerve palsy
Box 6.1 The causes of ‘claw hand’ deformities
Diagnostic plan
Treatment plan
1 Congenital contractures
2 Scar contractures
3 Dupuytren's contracture
4 Ischaemic contracture
5 Tendon lesions
6 Arthritis
7 Neurological lesions
6.8 Hand infections
Types of hand infection
Clinical assessment and diagnostic plan
Classification of treatment plan
1 Infected recent wounds
2 Subcutaneous infections
FIGURE 6.27 Finger infection1: nail fold suppuration (paronychia); 2: pulp space suppurative necrosis; 3: eponychium – cuticle; 4: pulp space with fascial septa
FIGURE 6.28 Pulp-space infection (Whitlow)Direct incision, adequate excision of slough and antibiotic treatment have reduced the need for older methods of extensive incision and irrigation.
3 Deep infections
FIGURE 6.29 ParonychiaA: raising the eponychium to release pus is sufficient in most cases; B: more severe infections require incision of the cuticle and removal of some or all of the nail
FIGURE 6.30 Surface markingsA: thenar fascial space; B: midpalmar fascial space
6.9 Nail disorders
TABLE 6.2 Nail changes in systemic disease
Common surgical disorders of the nail
History and physical examination
1 Subungual haematoma and melanoma
FIGURE 6.31 Anatomy of the nail1: visible nail; 2: nail covered by cuticle or eponychium; 3: lunule; 4: nail bed and germinal matrix; 5: terminal phalanx; 6: nail sulcus and lateral nail fold
2 Ingrown toenail
3 Paronychia
4 Periungual warts
5 Less common conditions
Diagnostic and treatment plans
1 Subungual haematoma and melanoma
2 Ingrown toenail
FIGURE 6.32 Correct (A) and incorrect (B) trimming of toenails
FIGURE 6.33 Digital nerve blockAdrenaline must not be added to local anaesthetic for a digital block.
3 Paronychia
FIGURE 6.34 Surgical treatment for ingrown toenailA: wedge excision procedure. The lateral third of the nail is avulsed. The nail bed is either excised, curetted or ablated with local phenol; B: Zadik's operation – the entire nail and nail bed, and the lateral nail folds, are excised
4 Periungual warts
5 Less common causes
6.10 Painful hip
Causes
Clinical assessment
FIGURE 6.35 Shortening at the hip jointA: Nelaton's line is drawn through the anterior superior iliac spine, the tip of the greater trochanter and the ischial tuberosity, and is a straight line when the femoral neck is of normal length; B: Bryant's triangle is constructed in a standing patient by drawing a horizontal line from the anterior superior spine to a vertical line drawn from the greater tuberosity. The vertical distance is reduced when shortening is at the hip or femoral neck.
FIGURE 6.36 Thomas' test for fixed flexion deformity of the hipLying supine, the flexion deformity of the right hip is masked by lordosis of the lumbar spine. When the sound hip is flexed, the deformity is revealed as the spine is flattened against the examination couch.
1 Osteoarthritis
FIGURE 6.37 Osteoarthritis of the right hip jointThe characteristic deformity is true shortening with external rotation of the lower limb. Flexion deformity may also be present.
2 Extrinsic causes of referred hip pain
3 Less common causes
Diagnostic plan
Treatment plan
6.11 Painful knee
Common causes
History and physical examination
FIGURE 6.38 Detection of fluid in the knee joint – medical aspect of the right legThe suprapatellar pouch is compressed with one hand while the other hand straddles the joint below and around the patella. Squeezing either hand transmits a fluid impulse.
FIGURE 6.39 McMurray's testThe McMurray test aims to induce jamming of the torn meniscus between the tibia and femur. The knee is flexed. The heel is grasped with the right hand and the knee steadied with the left hand. The knee is pressed medially and extended while the tibia is internally and externally rotated with the right hand.
FIGURE 6.40 Detection of cruciate ligament and meniscal damageThe tibial draw or glide test of cruciate ligament integrity. The examiner sits on the foot of the patient and with both hands, draws the tibia forward for anterior cruciate, and back for posterior cruciate damage.
1 Osteoarthritis and rheumatoid arthritis
2 Traumatic derangement of the knee
3 Bursitis
FIGURE 6.41 Swellings on the medial side of the knee1: prepatellar bursitis (housemaid's knee); 2: infrapatellar bursitis (clergyman's knee); 3: effusion in the suprapatellar pouch; 4: loose body; 5: pes anserinus bursa; 6: cyst of the medial meniscus; 7: Baker's cyst; 8: semimebranosus bursa; 9: popliteal aneurysm
4 Osteochondritis dissecans and osteonecrosis
Diagnostic plan
Radiology
Treatment plan
6.12 Painful foot
Clinical assessment
Common causes and clinical presentation
Pain in the forefoot (metatarsalgia)
FIGURE 6.42 Anterior flat footDropped transverse arch from collapse at the metatarsophalangeal joint is the most common cause of metatarsalgia and associated toe deformities. A: normal foot; 1: metatarsal; 2: proximal phalanx; B: anterior flat foot leading to hammer toe with callosity formation (3, 4); C: claw toe with flexion on both the proximal and distal interphalangeal joints
1 Anterior flat foot (with hallux valgus, hammer toe and claw toes)
FIGURE 6.43 Hallux valgusA: exostosis over the head of the first metatarsal with metatarsus varus; B: excision of the exostosis and excision of the proximal third of the first phalanx may correct the deformity (Keller's operation)
2 Stress or fatigue fracture (of the second or third metatarsal bones)
3 Morton's metatarsalgia
4 Plantar warts
FIGURE 6.44 Plantar wartA: papilloma with its clearly demarcated border; B: callous with its indistinct border
5 Ischaemic rest pain
Painful ankle and heel
1 Trauma
2 Overuse
FIGURE 6.45 Painful heel1: partial disruption of the lateral ligament of the ankle and tenosynovitis of the peroneal tendons; 2: subtalar arthritis with tenderness over the sinus tarsi just anterior to the lateral malleolus; 3: osteoarthritis of the ankle joint; 4: partial rupture of the Achilles tendon; 5: Achilles tendon bursitis; 6: calcaneal bursitis (tender heel pad); 7: plantar fasciitis
3 Spontaneous
Diagnostic plan
Treatment plan
Metatarsalgia
Painful ankle and heel
6.13 Swollen leg
Common causes
Acute swelling
Chronic swelling
Clinical features
Acute swelling
1 Deep venous thrombosis
Box 6.2 Risk factors for developing DVT
Abnormality/injury in the vein wall
Venous stasis
Hypercoagulability
2 Ruptured synovial cyst (pseudophlebitis)
3 Less common causes
Chronic swelling
1 Systemic disorders
FIGURE 6.46 Pitting oedemaChronic venous insufficiency is unlikely to be the cause of bilateral pitting oedema without other stigmata. A medical or systemic disorder is a much more common cause.
2 Chronic venous insufficiency
3 Lymphoedema
Diagnostic plan
Acute swelling
Chronic swelling
Box 6.3 Causes of lymphoedema
Primary
Secondary
Treatment plan
Acute swelling
Box 6.4 Management of DVT
Chronic swelling
Box 6.5 Instructions to patients for continued care of the leg damaged with chronic venous insufficiency
Box 6.6 Lymphoedema: objectives of treatment
6.14 Leg ulcer
Causes
History and physical examination
1 Chronic venous insufficiency (the ‘venous ulcer’)
FIGURE 6.47 Chronic venous stasis
2 Arterial insufficiency (the ‘arterial ulcer’)
3 Neuropathic ulcer (and often the ‘diabetic ulcer’)
FIGURE 6.48 Diabetic ulcer before and after WF10 treatment.Photographs of 56-year-old woman with DFU of 12 months' duration. A. neuropathic ulcer with positive probe to bone test before treatment; B. ulcer had healed after 1 cycle of WF10 treatment (photograph taken at week 5)
Box 6.7 The causes of neuropathic ulceration
Peripheral nerve lesions
Spinal cord lesions
4 Less common causes
Diagnostic plan
Treatment plan
Box 6.8 Local factors contributing to chronic leg ulceration
Box 6.9 Systemic factors contributing to chronic leg ulcer
1 Venous ulcer
Box 6.10 Compression treatment of varicose ulcers
Each morning
Each night
During the day
2 Arterial ulcer
3 The neuropathic ulcer and diabetic foot
FIGURE 6.49 Diabetic footThis patient had a neuropathic ulcer and necrotic toes but no arterial disease. The second and third metatarsals have been excised, together with all the necrotic tissue, in a ‘cake slice’ procedure. The wound was left open to heal by secondary intention, eventually giving a remarkably good functional result.
6.15 Varicose veins
Box 6.11 Caring for a diabetic foot
Common causes
Physiopathology
History
Examination
Diagnostic plan
Trendelenburg test
Venous groin cough impulse
Treatment plan
6.16 Limb ischaemia
Functional ischaemia – intermittent claudication
Causes
History
1 Occlusive peripheral vascular disease
2 Less common causes
Physical examination (see introduction, arterial examination)
Inspection
Palpation
Diagnostic plan
Treatment plan
Stop smoking – keep walking
Box 6.12 Management of peripheral vascular disease
Common causes
History and physical examination
General
Atherosclerotic large vessel disease
Other causes
Diagnostic plan
FIGURE 6.50a Intermittent embolic occlusionPatchy gangrene with palpable peripheral pulses suggests diabetes mellitus or emboli from a proximal aneurysm or plaque.
Treatment plan
FIGURE 6.50b Transfemoral angiography in two patients with rest painA: good run-off with a patent popliteal artery – suitable for surgical bypass; B: poor run-off – not suitable for reconstructive surgery
FIGURE 6.51 Percutaneous transluminal balloon or laser angioplastyA: a Grunzig balloon or laser light transmission fibre is passed along a vessel to the site of partial or complete occlusion; B: in balloon angioplasty the balloon is blown up to compress atheroma and recanalise the artery; C: laser light is delivered through an optical fibre at a wavelength that produces non-thermal destruction of atheromatous tissue
FIGURE 6.52 An excellent transtibial amputation stump with a long posterior flap myoplasty
Acute limb ischaemia
Common causes
Clinical features
Treatment plan
FIGURE 6.53a Acute ischaemic left footA: normal foot; B: foot with embolus
Raynaud's phenomenon
FIGURE 6.53b Aortic embolectomy using a Fogarty balloon catheter
Common causes
Clinical features
Treatment plan
Chapter 7 Abdominal and gastrointestinal problems
7.1 Introduction
History – analysis of abdominal pain
Location and migration
FIGURE 7.1 Migration of pain in common abdominal conditionsA: biliary pain – migration to below the top of the right scapula (‘wing sign’); B: perforated ulcer – down the right paracolic gutter; C: acute appendicitis – to the right iliac fossa; D: perforated diverticulitis – over the abdomen starting from the left iliac fossa; E: renal colic – from loin to groin
Onset and duration
Type and intensity
Radiation
Associated symptoms
Offsetting factors
Past history
Physical examination
Examination of the periphery
FIGURE 7.2 Physical signs of liver disease1: palmar erythema and ecchymoses; 2: xanthelasma, parotid enlargement; alcoholic facies; 3: spider naevi and gynaecomastia; 4: hepatomegaly; 5: splenomegaly (the main sign of portal hypertension); 6: dilated veins on the abdominal wall; 7: ascites; 8: testicular atrophy and loss of body hair; 9: pigmentation, ulceration and oedema; 10: proximal muscle wasting
Abdominal examination
FIGURE 7.3 Anterior surface markings of upper abdominal viscera
Anorectal examination
FIGURE 7.4 Posterior surface markings of abdominal visceraA: lung; B: pleura; C: kidney; D: pancreas; E: spleen
FIGURE 7.5 Regions of the abdomenA: epigastrium; B: right hypochondrium; C: lumbar region; D: periumbilical region; E: right iliac fossa; F: hypogastrium
FIGURE 7.6 Method of palpating the spleen
FIGURE 7.7 Palpable normal abdominal structures1: xiphoid process; 2: liver; 3: edge of rectus abdominis; 4: lower pole of right kidney; 5: caecum; 6: aorta; 7: ala of sacrum; 8: pregnant uterus; 9: full bladder; 10: sigmoid colon; 11: faecal loading
FIGURE 7.8 Shifting dullnessArea 1 is resonant when supine and dull in lateral position. Area 2 is dull when supine and resonant in lateral position.
TABLE 7.1 Typical physical characteristics of an enlarged liver, spleen and kidney
FIGURE 7.9 Rectal examinationDigital detection of a carcinoma of the rectum at about 10 cm from the anal verge. The characteristics on palpation are induration, elevation and ulceration. Blood may be seen on the glove after completion of the examination.
FIGURE 7.10 Anatomy of the anorectumThe anal canal extends from the anorectal ring, which is formed by the puborectalis, down to the anal verge, a distance of about 3 cm. 1: puborectalis muscle; 2: inferior haemorrhoidal plexus or cushion; 3: anal crypt; 4: dentate line; 5: interhaemorrhoidal groove; 6: anal verge; 7: external haemorrhoidal plexus; 8: external haemorrhoidal artery; 9: internal sphincter; 10: external sphincter
7.2 ‘Acute abdomen’ (acute abdominal surgical emergency)
Common causes of the ‘acute abdomen’
History and physical examination
1 Acute appendicitis with perforation (see also acute right iliac fossa pain)
2 Severe acute pancreatitis
TABLE 7.2 Comparison of perforated duodenal ulcer with acute pancreatitis
3 Perforated peptic ulcer
4 Diverticulitis with perforation
5 Strangulating intestinal obstruction
Box 7.1 Clinical features suggesting bowel strangulation
6 Vascular catastrophes
7 Ruptured ectopic pregnancy
8 Gastroenteritis
9 Less common causes
Diagnostic plan
Urine examination
Haematological examination
Biochemistry
Imaging techniques
FIGURE 7.11 Chest x-ray with gas under the diaphragm
FIGURE 7.12 Films of small bowel obstructionA: supine abdominal x-ray with dilated small bowel loops; B: erect abdominal x-ray with multiple air fluid levels (arrowed); C: typical ‘ladder’ pattern (arrowed) on supine abdominal x-ray
Treatment plan
1 Acute appendicitis with perforation
2 Severe acute (haemorrhagic) pancreatitis
Box 7.2 Acute pancreatitis: diagnostic plan
3 Perforated peptic ulcer
TABLE 7.3 Indicators of severity of acute pancreatitis (Glasgow system)
FIGURE 7.13 Common complications of acute pancreatitisA: pseudocyst of the pancreas in the lesser sac secondary to a leak from the main pancreatic duct; B: necrosis, haemorrhage and sepsis extends to the retroperitoneum. 1: inferior surface of the right lobe of the liver; 2: gall bladder; 3: stomach; 4: greater omentum; 5: transvese colon; 6: third part of the duodenum
Box 7.3 Significant risk factors in perforated duodenal ulcer
FIGURE 7.14 Simple closure of a perforated anterior duodenal ulcer (Roscoe-Graham method)Sutures are passed deep to the ulcer and tied over the omentum.
4 Perforated diverticulitis
5 Strangulating intestinal obstruction
6 Vascular catastrophes
FIGURE 7.15 Hartmann's procedureResection of the site of complicated diverticular disease is usually necessary if infection is to be controlled in patients with perforation. After excising the diseased segment, the risk of immediate bowel anastomosis in continuity is avoided by an end sigmoid colostomy (1) with closure of the rectal stump (2).
7 Ruptured ectopic pregnancy
8 Gastroenteritis
7.3 Acute upper abdominal pain
Causes
History
1 Acute gastritis and non-ulcer dyspepsia
2 Acute exacerbation of duodenal ulcer
3 Biliary ‘colic’ and acute cholecystitis
4 Acute (oedematous) pancreatitis
Examination
Gastritis and duodenal ulcer
Cholecystitis
Acute pancreatitis
Diagnostic plan
FIGURE 7.16 Pathology and natural history of gallstonesA: asymptomatic gallstones; B: biliary pain (chronic cholecysitis); B1: obstructive jaundice; B2: pancreatitis secondary to small stones; B3: ascending cholangitis; C: acute cholecystitis; C1: mucocele of gall bladder; C2: perforated empyema – with pericholecystic abscess; C3: free perforation; D: chronic cholecystitis; D1: cancer of gall bladder; D2: cholecysto-duodenal fistula and gallstone ileus
FIGURE 7.17 Acute cholecystitisAn acutely tender, palpable gall bladder is virtually diagnostic of acute cholecystitis. The gall bladder enlarges laterally rather than towards the umbilicus.
Haematological and biochemical examination
Radiology: plain erect film of chest and abdomen
Ultrasound and CT scanning
Radionuclide excretion scan
Gastrograffin swallow and meal
Late endoscopy and ERCP
Treatment plan
1 Acute gastritis and non-ulcer dyspepsia
2 Acute exacerbation of duodenal ulcer
3 Biliary ‘colic’ and acute cholecystitis
4 Acute (oedematous) pancreatitis
5 Less common causes
7.4 Acute right iliac fossa pain
Causes
History and physical examination
1 Acute appendicitis
TABLE 7.4 Comparison of clinical features of perforated pelvic appendicitis and gastroenteritis
FIGURE 7.18 Anatomy of the appendixThe caecum may be high (A) normal (B) or low (C) in position. The appendix may be free lying, paracaecal or retrocaecal, pre-ileal or postileal, or pelvic in position.
2 Acute mesenteric adenitis and acute Meckel's diverticulitis
3 Non-specific acute right iliac fossa pain
4 Gynaecological disorders
5 Urinary tract stone, infection or hydronephrosis
Diagnostic plan
Full blood count
Urine examination
Cervical swab and culture
Plain x-ray
Ultrasound
CT scan
Laparoscopy
HCG pregnancy test
Treatment plan
1 Acute appendicitis
2 Acute mesenteric adenitis and Meckel's diverticulitis
3 Non-specific acute right iliac fossa pain
4 Gynaecological disorders
5 Acute urinary tract stone, infection or hydronephrosis
6 Less common causes
7.5 Acute lower abdominal (pelvic) pain
Causes
History and physical examination
1 Diverticulitis
FIGURE 7.19 Complicated diverticulitisAcute abdomen due to: A: perforation of a pericolic abscess (purulent peritonitis); or B: perforation of an uninflamed diverticulum (faecal peritonitis).
2 Carcinoma of the colon
3 Pelvic appendicitis
4 Gynaecological disorders
TABLE 7.5 Acute abdominal pain in pregnancy
FIGURE 7.20 Sites of ectopic pregnancy implantation1: interstitial 4%; 2: isthmial 18%; 3: ampullary 55%; 4: abdominal cavity 1%; 5: fimbrial 20%; 6: ovarian 2%
Diagnostic plan
Full blood count, blood grouping and pregnancy test
Urine microscopy and analysis
Plain x-ray of the abdomen
Pelvic ultrasound
Laparoscopy
FIGURE 7.21 LaparoscopyThe uterus is stabilised per vaginum. The pelvis is inspected after insufflation of CO2 into the peritoneal cavity. An ectopic pregnancy is diagnosed here.
CT contrast study
Colonoscopy
Treatment plan
1 Diverticulitis
2 Carcinoma of the colon
3 Pelvic appendicitis
4 Gynaecological disorders
5 Less common causes
7.6 Chronic epigastric pain
Causes
History
1 Non-ulcer dyspepsia
TABLE 7.6 Features of the common causes of chronic epigastric pain
2 Gallstones and chronic cholecystitis
3 Duodenal ulcer
Box 7.4 Causes of combined upper and lower gastrointestinal symptoms
4 Gastric ulcer
5 Carcinoma of the stomach
TABLE 7.7 Comparison of the clinical features of duodenal and gastric ulcers
Examination
Diagnostic plan
Full blood examination
Ultrasound
Endoscopy
Contrast radiology
MRCP, CT cholangiography and ERCP
Treatment plan
1 Non-ulcer dyspepsia
2 Gallstones and chronic cholecystitis
Box 7.5 General instructions for relief of symptoms from gastritis or dyspepsia
3 Duodenal ulcer
FIGURE 7.22 Cholecystectomy – normal operative cholangiogramNo filling defects, normal duct anatomy and diameter, free flow of contrast into the duodenum, lower and upper reaches of duct well visualised.
4 Gastric ulcer
5 Carcinoma of the stomach
Box 7.6 Management of carcinoma of the stomach
FIGURE 7.23 Surgical management of carcinoma of the stomachA: antral tumours often present with vomiting and are managed by partial gastrectomy; B: body tumours present with chronic epigastic pain; total gastrectomy is usually required; C: tumours of the cardia present with dysphagia; oesophagogastrectomy required
FIGURE 7.24 Total gastrectomyTotal gastrectomy achieves best local control of disease. Reconstruction is by Roux-en-Y oesophagojejunostomy. The letters indicate the arrangement of structures before and after the gastrectomy and reconstruction.
6 Less common causes
Non-gastrointestinal causes
Gastrointestinal causes
FIGURE 7.25 Puestow's operationPuestow's operation (side-to-side Roux-en-Y pancreaticojejunostomy): for painful chronic pancreatitis with duct dilatation.
Box 7.7 Causes of postcholecystectomy syndrome
7.7 Chronic lower abdominal (pelvic) pain
TABLE 7.8 Postgastrectomy syndromes: management
Causes
History and physical examination
1 Chronic pelvic inflammatory disease
2 Pelvic congestion syndrome
3 Endometriosis
4 Functional bowel disorders and diverticular disease
Diagnostic plan
Full blood examination
Radiological examination
Microbiological examination
Laparoscopy
Treatment plan
1 Pelvic inflammatory disease
2 Pelvic congestion syndrome
3 Endometriosis
4 Functional bowel disorders and diverticular disease
5 Less common causes
FIGURE 7.26 Drainage of pelvic abscessA: An artery forcep is guided over the index finger through the point of maximum softening in the anterior rectal wall.
7.8 Bowel obstruction
Initial assessment: small or large bowel obstruction?
Box 7.8 Management plans in small bowel obstruction
Small bowel obstruction
Common causes
History
1 Adhesive obstruction
FIGURE 7.27 Clinical presentations of small bowel obstruction depend upon the level and cause of obstructionA: high obstruction (adhesive): vomiting early and profuse, pain atypical or absent, distention minimal, x-ray may be negative; B: distal small bowel, strangulated hernia: colicky pain, distension, vomiting; local symptoms not always prominent; C: obstructing carcinoma, right colon, distal small bowel obstruction
2 Hernias
3 Malignancies
4 Sigmoid diverticulitis and intraperitoneal abscess
5 Gallstone ileus and enteroliths
Examination
FIGURE 7.28 Intussusception1: possible foci for intussusception and diagrammatic representation of mechanism; 2: barium enema of the small bowel ‘into’ colon intussusception; 3: pathological specimen illustrating C – colon, I – intestine and A – appendix
Diagnostic plan
Haematological and biochemical examination
Radiology
FIGURE 7.29 Complicated diverticular diseaseSmall bowel obstruction secondary to diverticulitis with small bowel adherence to sigmoid colon affected by diverticulitis.
FIGURE 7.30 Diagrammatic depiction of radiological features of small bowel obstructionA: erect film; B: supine film
Treatment plan
Nasogastric drainage and decompression
Resuscitation
Box 7.9 Extracellular fluid replacement in small bowel obstruction*
Volume of replacement fluid
Composition of replacement fluid
Rate of replacement
Surgical intervention
Management of other causes
Large bowel obstruction
Common causes
FIGURE 7.31 Large bowel obstructionA: often the ileocaecal valve prevents retrograde decompression into the small bowel, creating a closed loop obstruction; B: alternatively, with spontaneous decompression into the small bowel the presentation is less acute and the danger of caecal perforation is less
History and physical examination
1 Colonic carcinoma
2 Sigmoid or caecal volvulus
3 Diverticular disease
4 Colonic pseudo-obstruction
5 Faecal impaction
FIGURE 7.32 Sigmoid volvulusA: diagram of sigmoid volvulus: direction of twist is usually anticlockwise. B: plain abdominal x-ray of sigmoid volvulus showing a distended loop arising from the pelvis; on sigmoidoscopy the site of obstruction can be seen at about 15–20 cm from the anal verge
Diagnostic plan
Treatment plan
1 Colonic carcinoma
2 Sigmoid or caecal volvulus
3 Diverticular obstruction
4 Colonic pseudo-obstruction
5 Faecal impaction
7.9 Abdominal mass
General assessment
1 Confirm a mass is present
2 Categorise the mass
FIGURE 7.33 Upper abdominal masses1: enlarged liver; 2: Riedel's lobe; 3: carcinoma of the right colon; 4, 5: gall bladder; 6: rounder lower poles of both kidneys; 7: abdominal aortic aneurysm; 8: splenomegaly; 9: pseudocyst of the pancreas
FIGURE 7.34 The life cycle of the hydatid parasiteA: Primary host – dog. After eating sheep offal (liver, lung) containing hydatid cysts, the scolices pass into the small intestine and grow into the adult tapeworm Echinococcus granulosus. The eggs produced by the terminal segments are shed and passed in canine faeces. B: Secondary hosts – sheep and humans. Ova are ingested, the chitinous enveloped is dissolved by acid and pepsin in the stomach. After absorption, ova pass via the portal blood to the liver and grow into adult hydatid cysts containing scolices.
Right upper quadrant mass
Common causes
History and examination
1 Single mass in the liver
2 Mucocele of the gall bladder
3 Right renal swelling
4 Carcinoma of the right colon
Diagnostic plan
Treatment plan
FIGURE 7.35 The segmental anatomy of the liver displayed ex vivoRight hepatectomy: segments v, vi, vii, viii; left hepatectomy: segments ii, iii, iv; right lobectomy: segments iv, v, vi, vii, viii; left lobectomy: segments ii, iii; segments v, vi, vii, viii are supplied by the right hepatic artery, segments i, ii, iii, iv are supplied by the left hepatic artery.
FIGURE 7.36 Liver hydatidA: adventitia derived from the host; B: laminated chitinous layer; C: germinal layer – which gives rise to brood capsules containing scolices. Daughter cysts float free within the main cyst, together with detached brood capsules and scolices (hydatid sand).
Hepatomegaly
Common causes
Smooth regular liver enlargement
Irregular or nodular liver enlargement
Symptoms and signs
Box 7.10 Causes of massive hepatomegaly and splenomegaly
Hepatomegaly
Splenomegaly
Diagnostic and treatment plans
Haematological tests
Liver function tests
Scanning
Biopsy
Left upper quadrant mass
Common causes
History and examination
Diagnostic plan
Treatment plan
Splenomegaly
Common causes
History and examination
Diagnostic and treatment plans
Combined liver and spleen enlargement
Common causes
History and examination
Diagnostic and treatment plans
Epigastric mass
Common causes
History and examination
Gastrointestinal masses
Retroperitoneal mass
Abdominal aortic aneurysm
Diagnostic plan
Incidental imaging findings (‘incidentaloma’)
Treatment plan
Right iliac fossa mass
Causes
History and examination
FIGURE 7.37 Excision and replacement of abdominal aortic aneurysm with a synthetic graftThe adventitia of the aneurysmal wall is closed over the graft.
Diagnostic plan
Treatment plan
Less common causes
Left iliac fossa mass
Causes
History and examination
Diagnostic plan
Treatment plan
Less common causes
Abdominal swellings arising from the pelvis
Common causes
History and examination
FIGURE 7.38 Lower abdominal masses1: full urinary bladder; 2: ovarian cyst; 3: fibromyomas of uterus; 4: tender mass of appendiceal abscess; 5: pregnant uterus; 6: tender mass of diverticulitis
Diagnostic plan
Treatment plan
7.10 Abdominal distension
Common causes
History and examination
1 Fat
2 Pregnant uterus (fetus)
3 Accumulation of gastrointestinal gas (flatus)
4 Faecal impaction (faeces)
5 Ascites or encysted liquid (fluid)
Causes of ascites (free intraperitoneal fluid)
FIGURE 7.39 Collateral venous bloodflow on the anterior abdominal wallA: portal venous obstruction with ascites; B: inferior vena caval obstruction
Causes of encysted fluid
Diagnostic plan
Treatment plan
7.11 Retrosternal pain and heartburn
Causes
History
1 Ischaemic heart disease – angina pectoris
2 Reflux oesophagitis and hiatus hernia
3 Diffuse oesophageal spasm
4 Musculoskeletal or chest wall pain
Examination
Diagnostic plan
Haematological examination
Electrocardiography
Organ imaging and endoscopy
FIGURE 7.40 Oesophagus hiatus herniaA: sliding hernia – front (A1) and side (A2) views; B: paraoesophageal or rolling hernia. Reflux with oesophagitis occurs in about 50% of sliding hernias but is rare in rolling hernia where the main danger is intrathoracic incarceration and strangulation of the stomach.
Manometry
Treatment plan
1 Ischaemic heart disease – angina pectoris
2 Reflux oesophagitis and hiatus hernia
Box 7.11 General instructions for reflux oesophagitis with heartburn (hiatus hernia)
Box 7.12 Indications for anti-reflux oesophageal surgery
FIGURE 7.41 Nissen fundoplicationA: initially the hernia is reduced and the defect in the diaphragmatic hiatus is narrowed with sutures; B: the fundus is wrapped around the distal oesophagus down which has been passed a large bougie (50F); C: the wrapped fundus is sutured in place to produce a valve in the lower oesophagus from the pressure of the surrounding stomach, therefore preventing reflux and herniation
3 Diffuse oesophageal spasm
4 Musculoskeletal or chest wall pain
5 Less common causes
7.12 Dysphagia
Causes
History
1 Foreign body
2 Reflux oesophagitis and benign stricture
3 Carcinoma of the oesophagus
4 Achalasia and diffuse oesophageal spasm
Signs
Diagnostic plan
Haematological examination
Radiology
FIGURE 7.42 Contrast radiological features of achalasiaA: dilated oesophagus; B: rat-tail narrowing of the distal oesophagus; C: no gastric air bubble. Endoscopy demonstrates no organic stricture.
Endoscopy and biopsy
Manometry
Treatment plan
1 Foreign body
2 Reflux oesophagitis and benign stricture
FIGURE 7.43 Oesophageal dilatation of benign strictureOesophageal dilatation of benign stricture is performed using A: the Eder-Puestow (graded size metal olives); or B: Celestin dilators (stepped dilators in two sizes). Initially a flexible guide wire is passed under vision through the stricture into the stomach. The endoscope is then removed, leaving the guide wire in place and the dilators are passed over the wire.
3 Carcinoma of the oesophagus
Box 7.13 Management of benign stricture secondary to reflux
FIGURE 7.44 Palliative treatment of advanced carcinoma of the oesophagus in a poor-risk caseA: endoscopic intubation using an Atkinson or Celestin tube; B: neodymium:yttrium-argon laser photocoagulation
TABLE 7.9 Management of carcinoma of the oesophagus
4 Achalasia and diffuse oesophageal spasm
FIGURE 7.45 Ivor Lewis-Tanner oesophagogastrectomy for carcinoma of the middle and distal third of oesophagus, and gastric cardiaThe stomach is mobilised on the right gastric (1) and right gastroepiploic arteries (2). The left gastric artery (3) and short gastric arteries (4) are divided. After thoracotomy and resection of the tumour (5) the stomach is passed up into the right chest and its fundus (A) anastomosed to the oesophagus. The gastric resection line (B) has been closed primarily. A pyloroplasty aids gastric emptying.
5 Less common causes
FIGURE 7.46 Cricopharyngeal achalasia with pharyngeal (Zenker's) pouchPharyngeal pouch is a pulsion diverticulum secondary to high pharyngeal pressure above spasm of the cricopharyngeous muscle. A: Lateral view shows the pouch coming from between the cricopharyngeal and thyropharyngeal portions of the inferior constrictor. B: Posterior view shows Killian's dehiscence, an area of muscle deficiency and weakness through which the pouch develops. The pouch usually extends to the left side of the neck. As it enlarges, the opening comes in line with the oesophageal axis, making endoscopy potentially hazardous. C: Lateral image of contrast study.
FIGURE 7.47 Para-oesophageal hiatus herniaA: Para-oesophageal hiatus hernia. B: Volvulus of the stomach in a para-oesophageal hiatus hernial sac. The stomach has rotated on its long axis (organo-axial volvulus). This produces an acute kink in the distal oesophagus that causes dysphagia, bloating without vomiting, and prevents the passage of a nasogastric tube. An air–fluid level is seen in the chest behind the heart on plain x-ray.
7.13 Weight loss
Common causes
History
1 Depression
2 Abdominal malignancy
3 Diabetes mellitus
4 Thyrotoxicosis
5 Chronic infections
6 Malabsorption
Signs
1 Depression
2 Abdominal malignancy
3 Diabetes mellitus
4 Thyrotoxicosis
Diagnostic plan
Haematological and biochemical examination
Urine analysis and culture
Organ imaging and endoscopy
Weight gain
7.14 Vomiting
Box 7.14 Common causes of weight gain
Causes
History
1 Duodenal ulcer
2 Carcinoma of the pyloric antrum
3 Functional bowel disease and psychogenic vomiting
TABLE 7.10 Comparison of benign and malignant gastric outlet obstruction
4 Drug-induced vomiting
Examination
Box 7.15 Drugs that can cause chronic vomiting
Diagnostic plan
Urinalysis
Haematology
Biochemistry of urine and blood
Radiological investigation
Treatment plan
Nasogastric suction
TABLE 7.11 Pyloric stenosis: stages of fluid and electrolyte disorders
Correction of extracellular fluid loss and hypokalaemic alkalosis
Surgical intervention
5 Less common causes
FIGURE 7.48 GastrectomyB1 = Billroth gastrectomy, B2 = Billroth II (polya) gastrectomy and TG = total gastrectomy and Roux-en-Y oesophagojejunostomy
7.15 Jaundice
Causes
History
1 Stone in the bile duct
2 Carcinoma of the head of the pancreas
3 Alcoholic liver disease
4 Drug-induced jaundice
5 Viral hepatitis
Examination
Diagnostic plan
Haematology
Biochemistry
Diagnostic and interventional imaging: ultrasound and CT
Liver biopsy
FIGURE 7.49 Sonolucent gall bladderMost gallstones are radiolucent radiologically but, with ultrasound, they appear as mobile, shadowing, echogenic foci in a sonolucent gall bladder.
Endoscopic retrograde cholangiopancreatography
Percutaneous cholangiography
Treatment plan
FIGURE 7.50 Endoscopic sphincterotomyERCP diathermy sphincterotomy before basket removal of a stone or insertion of a stent to bridge an obstruction.
1 Stone in the bile duct
Box 7.16 Management of bile duct stone in four clinical situations
Incidental finding at cholecystectomy (operative cholangiography)
Resolving jaundice
Persistent jaundice
Suppurative cholangitis
2 Carcinoma of the head of the pancreas
Box 7.17 Management of carcinoma of the head of pancreas
FIGURE 7.51 Palliative double bypass for obstructing carcinoma of the pancreas or distal bile ductThe procedures performed are A: Roux-en-Y choledochojejunostomy to control jaundice; and B: gastrojejunostomy to prevent later symptoms from duodenal obstruction.
Less common causes
FIGURE 7.52 Whipple's procedureWhipple's operation (pancreatoduodenectomy) for resectable carcinoma of the head of the pancreas or ampullary tumours. The non-shaded areas are resected, vagotomy is performed and intestinal continuity is reestablished by A: invaginating the pancreas into the terminal jejunum; B: anastomosing the bile duct to the side of the jejunum; and C: completing a gastrojejunostomy.
Intrahepatic obstruction
7.16 Haematemesis and melaena (upper gastrointestinal haemorrhage)
Causes
Box 7.18 Principles of management of bleeding ulcer
History
1 Duodenal and gastric ulcer
2 Oesophageal varices
Box 7.19 Causes of portal hypertension
Intrahepatic
Presinusoidal
3 Haemorrhagic antral gastritis
4 Mallory-Weiss syndrome
Examination
TABLE 7.12 Grading of severity of liver disease (modified Child's criteria – according to Pugh)
Diagnostic plan
Haematological assessment
Endoscopy
Treatment plan
General measures
High-risk patients
1 Duodenal and gastric ulcer
2 Oesophageal varices
3 Haemorrhagic antral gastritis
FIGURE 7.53 Surgery for a bleeding duodenal ulcerA: the duodenum is opened and the bleeding point is overswen in the base of the ulcer; B: pyloroplasty is completed by closing the longitudinal incision transversely. The operation is completed by performing a total truncal vagotomy.
4 Mallory-Weiss syndrome
FIGURE 7.54 Ballon tamponade using the quadruple lumen Minnesota tubeThe four lumina are A: nasopharyngeal aspiration tube; B: port for the gastric balloon; C: gastric aspiration tube; D: port and pressure gauge for the oesophageal balloon; and E: traction (0.5 kg).
Box 7.20 General management of patients with bleeding varices
5 Less common causes
7.17 Acute lower gastrointestinal (colorectal) haemorrhage
Causes
History and examination
1 Diverticular disease
2 Colonic angiodysplasia
3 Ischaemic colitis
FIGURE 7.55 Diverticular haemorrhage as a cause of colonic haemorrhageA: the diverticulum appears through the defect in the inner circular muscle through which passes the vasa recta; the artery is often stretched over the fundus of the diverticulum; B: erosion of the vessel can occur beneath stercoral ulceration produced by a faecolith
4 Colorectal polyps
5 Colorectal cancer
6 Other causes
Diagnostic and treatment plans
Haemodynamically stable
Haemodynamically unstable
FIGURE 7.56 Diathermy snare colonic polypectomyA: the snare is tightened on the neck of the polyp; B: current is applied while the polyp is continuousy moved to avoid a local full thickness burn; C: the resected polyp is sucked against the tip of the colonoscope for removal
7.18 Iron deficiency anaemia
Common causes
History and examination
Diagnostic plan
Oesophagogastroduodenoscopy
Colonoscopy
Radionuclide scan and CT angiography
CT scan abdomen and pelvis with contrast
Treatment plan
FIGURE 7.57 Right hemicolectomy1: superior mesenteric artery; 2: middle colic artery; 3: right colic artery; 4: ileocolic artery. Dotted line represents line of resection
7.19 Anorectal bleeding
Common causes
FIGURE 7.58 Anorectal bleedingA: blood coming from the rectum is persistent, associated with tenesmus, and due to polyps, cancer or proctitis; B: bleeding from haemorrhoids in the anal canal is periodic, painless, profuse and bright red; C: bleeding from the anal verge is small in amount, bright red, seen only on the toilet paper and due to fissure or skin tag. 1: anorectal ring; 2: dentate line; 3: anal verge
History
1 Haemorrhoids
2 Carcinoma of the rectum
3 Anal fissure
4 Proctitis
Examination
FIGURE 7.59 Classification of haemorrhoids into four degrees based on the severity of the diseaseFirst-degree haemorrhoids presents with bleeding; second-degree haemorrhoids prolapse but return spontaneously; third-degree must be manually returned; and fourth-degree are permanently prolapsed.
Diagnostic plan
Treatment plan
1 Haemorrhoids
2 Carcinoma of the rectum and anus
FIGURE 7.60 Barron band ligation of internal hemorrhoidsWorking through a proctoscope a rubber band (A) is dislodged from the cylinder to encircle the neck of an internal haemorrhoid (B).
FIGURE 7.61 Operative procedures performed for carcinoma of the distal large bowelA: anterior resection with primary anastomosis for middle- and upper-third rectal lesions; B: abdominoperineal resection with end sigmoid colostomy for distal-third rectal carcinoma. 1: inferior mesenteric artery; 2: left colic branch; 3: sigmoid branch; 4: superior rectal artery
3 Anal fissure
4 Proctitis
5 Less common causes
7.20 Altered bowel habit (constipation)
FIGURE 7.62 Forms of presentation of large bowel cancerA: right colon cancer usually presents with anaemia, often associated with mild dyspepsia or a mass; B: left colon cancer presents with altered bowel habit associated with varying degrees of pain from partial obstruction; C: cancer of the sigmoid colon sometimes presents with an acute abdomen from large bowel obstruction or perforation; D: distal large bowel and rectal cancers usually present with rectal bleeding associated with varying degrees of hypogastric pain and tenesmus
FIGURE 7.63 Common causes of tenesmusA: haemorrhoids; B: carcinoma of the rectum; C: rectal prolapse; D: faecal impaction; E: inflammatory bowel disease
Causes
History
1 Colorectal cancer
2 Functional bowel disorders
3 Psychiatric disorders
Box 7.21 Drugs that cause constipation
4 Drug-induced constipation
Examination
Diagnostic plan
Haematology
Sigmoidoscopy
Colonoscopy
Whole gut transit studies
Treatment plan
1 Colorectal cancer
Box 7.22 Common therapeutic agents used in the management of constipation
Hydrophilic bulking agents
Irritant purgatives
Suppositories
Enemas
2 Functional bowel disorders
3 Psychiatric disorders
4 Drug-induced constipation
5 Less common causes
High-fibre diet
7.21 Diarrhoea
Causes
History
1 Functional bowel disorders
TABLE 7.13 Diarrhoea: clinical features assisting the diagnosis
Box 7.23 Cardinal features of the syndrome of functional bowel disease
2 Inflammatory bowel disease
3 Colorectal cancer
Examination
Rectal examination – proctoscopy or rigid sigmoidoscopy
TABLE 7.14 Pathological features of inflammatory bowel disease
Diagnostic plan
TABLE 7.15 Radiological features of inflammatory bowel disease
Treatment plan
1 Functional bowel disorders
2 Inflammatory bowel disease
FIGURE 7.64 Diagrammatic representation of toxic megacolonThere is dilatation, gas in the bowel wall and loss of haustra in the transverse colon.
FIGURE 7.65 Segmental colectomyA: transverse colectomy for carcinoma of the transverse colon with division of the left main branch of the middle colic artery; B: left hemicolectomy for carcinoma of the descending colon, with ligation of the left colic artery
Box 7.24 Indications for surgery in ulcerative colitis
Acute disease
Chronic disease
3 Carcinoma of the colon
FIGURE 7.66 Surgical procedures used for ulcerative colitisA: protocolectomy and Brooke ileostomy; used mainly for emergency surgery and for older patients; B: ilioanal J-pouch with preservation of anal sphincters, used mainly as an elective operation in younger patients; contraindicated in Crohn's disease
Box 7.25 Indications for surgery in Crohn's disease
4 Less common causes
Box 7.26 Drugs that cause chronic diarrhoea
7.22 Acute anal pain
Causes (see Fig 7.67)
History
1 Perianal haematoma
FIGURE 7.67 Common causes of acute anal painA: perianal haematoma; B: anal fissure; C: strangulated haemorrhoids; D: perianal abscess
2 Anal fissure
3 Complicated haemorrhoids
4 Perianal abscess
Examination
FIGURE 7.68 Anatomical location of perianal abscessesA: perianal; B: intermuscular; C: supra-levator
FIGURE 7.69 Natural history of anal fissureA: acute fissure; B: chronic fissure – weeks later; C: chronic fissure – months later. 1: hypertrophied anal papilla; 2: sentinal pile; 3: subcutaneous fistula
Diagnostic plan
Treatment plan
1 Perianal haematoma
2 Anal fissure
3 Complicated haemorrhoids
4 Perianal abscess
5 Less common causes
7.23 Anal pruritus
FIGURE 7.70 Causes of anal or perianal dischargeA: advanced haemorrhoids; B: advanced carcinoma of the rectum (or villous adenoma); C: faecal impaction; D: pruritus ani; E: perianal fistula
FIGURE 7.71 Perianal discharge observed in left lateral position1: pruritus ani with exudation; 2: haemorrhoids; 3: perianal fistula; 4: furunculitis with chronic sinus formation
Common causes (see above)
History and examination
Box 7.27 Risk factors for pruritus ani
Diagnostic plan
Treatment plan
Measures to improve bowel habits
Local toilet hygiene
Box 7.28 Management of anal irritation
Diet
Hygiene
Local treatment
Remove irritants
Encourage healing
Surgery
7.24 Anorectal lump
Common causes
History and examination
1 Haemorrhoids
2 Rectal prolapse
FIGURE 7.72 Anal lumpsA: prolapsing lumps; 1: second- and third-degree haemorrhoids; 2: rectal polyp; 3: rectal prolapse; 4: hypertrophied anal papilla; B: persistent lumps; 1: condylomata; 2: skin tag; 3: carcinoma of the anal canal; 4: fourth-degree haemorrhoids; 5: perianal haematoma; 6: perianal fistula; 7: perianal abscess
FIGURE 7.73 Rectal prolapse1a: puborectalis spasm (anismus) with ineffective straining; 1b: treatment by division of the puborectalis muscle; 2: anteriror rectal wall descent with solitary rectal ulcer from abrasion of the apex; 3a: rectal prolapse; 3b: rectal prolapse treated by rectopexy (Ripstein repair)
3 Skin tags, hypertrophied anal papilla
4 Anal fistula
5 Carcinoma of the anus
Diagnostic plan
Treatment plan
1 Haemorrhoids
2 Anal fistula
3 Rectal prolapse
4 Skin tags and hypertrophied anal papilla
5 Carcinoma of the anus
7.25 Faecal incontinence
Common causes
History and examination
1 Anal sphincter injury
FIGURE 7.74 Anorectal incontinenceA: neurogenic and idiopathic incontinence; B: incontinence associated with rectal prolapse; C: traumatic incontinence; D: incontinence secondary to rectal Crohn's disease; E: rectovaginal fistula (pseudo-incontinence)
Box 7.29 Useful questions to ask for faecal incontinence
2 Constipation with overflow incontinence (see Ch 7.20)
3 Dietary factors and drugs
4 Idiopathic faecal incontinence
5 Neurological disease
6 Congenital disorders
Diagnostic plan
Treatment plan
Basic strategies
Pharmacotherapy
Sphincter reconstruction
Sacral neuromodulation (SNM)
Other procedures
7.26 Pneumaturia
Common causes
History and examination
Diagnosis
FIGURE 7.75 DiverticulitisPartial obstruction of the sigmoid colon by diverticulitis and a peridiverticular phlegmon. Obstructive symptoms are produced by extrinsic compression.
Treatment plan
FIGURE 7.76 Vesicocolic fistulaThe fistula is usually short, arising from a sigmoid peridiverticular abscess that has discharged into the bladder.
7.27 Anal fistula
Causes
History and examination
1 Anal fistula – crytoglandular origin
FIGURE 7.77 Perianal abscess leading to perianal fistula1: anal gland; 2: anal gland abscess; 3a, b: fistulous tract left after drainage; 4: established fistula
2 Anal fistula – Crohn's disease
FIGURE 7.78 Goodsall's ruleA: anterior fistulas open directly into an adjacent end crypt; B: posterior fistulas usually take a curved path to open into a midline posterior crypt; C: a horseshoe fistula may also have an anterior component
3 Malignant anal fistula
Diagnostic plan
Treatment plan
FIGURE 7.79 Anal fistulas1: anorectal (supraphincteric); 2: intermuscular; 3: high transsphincteric; 4: low transsphincteric; 5: subcutaneous (superficial), with anal fissure
1 Anal fistula – crytoglandular origin
FIGURE 7.80 Probing a fistula at operationA, B: the tract is gently probed to find the internal opening; C: the fistula is laid open by deroofing over the probe
2 Anal fistula – Crohn's disease
3 Malignant anal fistula
Chapter 8 Groin, scrotum and abdominal wall problems
8.1 Introduction
History
Physical examination
Examination: patient standing
Box 8.1 Risk factors for inguinal hernia
FIGURE 8.1 Surgical anatomy of the groinA: anterior superior iliac spine; B: external ring; C: femoral canal; D: femoral artery and vein; E: internal ring; F: inguinal ligament; G: abdominal crease
FIGURE 8.2 Examination: patient standingA: saphena varix; B: varicocele
FIGURE 8.3 Saphena varixPercussion over the saphenous vein in the thigh produces a transmitted impulse in the varix above.
Box 8.2 Typical features of a hernia
1 Is a hernia present? (Box 8.2)
2 Is the hernia inguinal or femoral?
FIGURE 8.4 Inguinal or femoral hernia?A: femoral hernia is sited below and lateral to the pubic tubercle (B); C: inguinal hernia appears at the external ring above and medial to the pubic tubercle
Examination: patient supine
3 Is the hernia reducible?
4 Is the hernia strangulated?
5 Is a scrotal lump present?
6 Can one get above the scrotal lump?
FIGURE 8.5 Scrotal examinationA: sequential examination of 1: testis; 2: tunica vaginalis; 3: epididymis; 4: cord; 5: superficial inguinal ring; B: palpation of epididymis
7 Is the lump arising from the testis or epididymis?
8 Does the lump arise from the coverings or from appendages?
General examination
8.2 Inguinoscrotal lumps
Scrotal lumps
Causes
Acute scrotal swelling
FIGURE 8.6 Scrotal lumpsA: acute: 1: torsion; 2: epididymo-orchitis, 3: torsion of the hydatid of Morgagni; B: chronic: 1: hydrocele; 2: haemoatocele; 3: epididymal cyst; 4: chronic epididymo-orchitis; 5: testicular neoplasm; 6: varicocele
Chronic scrotal swelling
Clinical assessment, diagnostic and treatment plans
Acute scrotal swelling
1 Torsion of testis
2 Acute epididymo-orchitis
3 Torsion of the hydatid of Morgagni
4 Traumatic haematocele
Chronic scrotal swellings
1 Hydrocele
2 Haematocele
3 Epididymal cysts
4 Chronic epididymo-orchitis
5 Testicular neoplasm
FIGURE 8.7 Presentation of testicular neoplasm1: painless lump in the testis; 2: ‘flash-fire’ presentation mimicking acute epididymo-orchitis; 3: large secondary hydrocele with occult primary – especially in younger patients; 4: secondary disease from occult primary
6 Varicocele
Groin and inguinoscrotal lumps
Causes
Clinical assessment and treatment plan
FIGURE 8.8 Varicocele1: absent valves in the left testicular vein lead to venous hypertension; 2: high ligation of the testicular vein; 3: inguinal canal and deep ring; 4: varicose pampiniform plexus
FIGURE 8.9 Inguinoscrotal lumpsA: inguinoscrotal hernia; B: varicocele; C: lipomatosis of the cord; D: encrysted hydrocele of the cord or canal of Nuck; E: testicular neoplasm with spread along the cord
Box 8.3 Clinical features of inguinal hernia
Indirect hernia
Direct hernia
FIGURE 8.10 Inguinal hernia: direct or indirect?1: indirect hernia runs within the spermatic cord through the external ring; 2: direct hernia emerges through the external ring behind the cord
FIGURE 8.11 Indirect inguinal herniaClassification A1–2: hernia magna; B1–2: funicular hernia; C1–3: sliding hernia (hernia-en-glissade). The sac consists in part of the serosal covering of the bowel, in this case sigmoid colon.
FIGURE 8.12 Strangulated indirect inguinal herniaA tense, tender, irreducible hernia with loss of the cough impulse. Bowel obstruction with early vomitting, abdominal (as well as local) pain, extracellular fluid loss and systemic toxicity.
FIGURE 8.13 Femoral herniaA: surface marking of femoral hernia; B: anatomy; 1: symphysis pubis; 2: lacunar ligament; 3: femoral hernia; C: large femoral hernia extending above inguinal ligament
FIGURE 8.14 Richter's herniaA variant of strangulated hernia seen most commonly with a femoral hernia. Part of the circumference of the bowel is entrapped.
Management plan
FIGURE 8.15 Inguinal herniorrhaphy1, 2: exposure of the inguinal canal; 3: opening canal; 4: dissection of the hernial sac from the cord; 5: excision of the hernial sac; 6: repair of the deep ring and posterior wall of inguinal canal
8.3 Abdominal wall problems
The umbilicus
Umbilical discharge
Common causes
Clinical features and treatment plan
1 Omphalitis
2 Embryological remnants
3 Intertrigo, umbilical concretions or granulomas
4 Ulcerated malignant nodule (Sister Mary Joseph's nodule)
5 Pilonidal sinus
Umbilical swellings and defects
Causes
Clinical features and treatment plan
1 Congenital abdominal wall defects
2 Umbilical hernias
FIGURE 8.16 Umbilical herniaA: The normal umbilicus lies over the linea alba, with the rectus abdominus muscle on either side. B: Primary umbilical hernias protrude through the umbilical scar. C: Acquired umbilical hernias are periumbilical so that the umbilical side of the skin dimple becomes an eccentric crescent-shaped slit.
Swellings of the abdominal wall
Causes
Clinical features and treatment plan
1 Subcutaneous and intramuscular swellings
FIGURE 8.17 Mayo repair of large umbilical herniaA: excision of sac; B: transverse repair using overlap
2 Abdominal wall hernias
FIGURE 8.18 Sites of ventral hernias1: epigastric; 2: incisional; 3: Spigelian; 4: umbilical
FIGURE 8.19 Diaphragmatic hernia1: foramen of Morgagni – between the sternal and costal slips of the diaphragm; 2: oesophageal hiatus; 3: foramen of Bochdalek
Chapter 9 Urogenital Problems
9.1 Introduction
History
Physical examination
Box 9.1 Lower urinary tract symptoms
Storage symptoms
Voiding symptoms
Diagnostic tests
FIGURE 9.1 Palpation of right kidney
9.2 Loin Pain
FIGURE 9.2a Cystoscopy and ureteric catheterisationA: tip of cystoscope with elevating bridge; B: trigone of bladder; C: ureteric oriface; D: interureteric bar
FIGURE 9.2b Normal right ureteric orifice as seen on cystoscopy
FIGURE 9.2c Right ureteric orifice with guidewire in situ
Causes
FIGURE 9.3 Radiation of ureteric ‘colic’Typically, a continuous severe pain that radiates from the renal angle and flank to the abdomen, parallel to the inguinal ligament, to the base of the penis and into the scrotum.
Clinical assessment
1 Renal pain (ureteric colic)
2 Pain referred from the ovary or other abdominal viscera
Box 9.2 Features of ureteric colic
3 Musculoskeletal pain
4 Less common causes
Diagnostic plan
Box 9.3 Types of urinary calculi
Treatment plan
Ureteric colic
FIGURE 9.4a Ureteric stoneRight-sided obstruction from stone causing hydronephrosis.
FIGURE 9.4b CT stone coronal view of a vesicoureteric junction (VUJ) stone
FIGURE 9.4c IVP demonstrating proximal ureteric stone
Management of urinary calculi
Box 9.4 Indications for removal/disruption of symptomatic renal or ureteric stone
FIGURE 9.4d URS/ureteroscopic view of stone
FIGURE 9.4e Extracorporeal shock wave lithotripsy (ESWL)
Management of recurrent urinary calculi
9.3 Painless Haematuria
Causes
Clinical assessment and urine microscopy
FIGURE 9.5 Common causes of painless haematuriaA: renal tumour; B: tuberculosis (now very uncommon); C: transitional cell tumour; D: engorged prostatic veins
Diagnostic and treatment plan
FIGURE 9.6a Staging of bladder tumourT1: confined to lamina propria; T2: invading the muscle wall of the bladder; T3: extending through the bladder wall; T4: involving other organs or nodal spread
FIGURE 9.6b Endoscopic photo of TCC
9.4 Lower urinary tract symptoms
Common causes
Clinical features and diagnostic plan
Urinary tract infections
Lower urinary tract infections
Upper urinary tract infections
Storage LUTS
Urinary tract pain
Voiding LUTS
9.5 Poor Urinary Stream
Common causes
Symptoms and signs
FIGURE 9.7a Effect of urinary obstructionA: obstruction effect; 1: prostatic hyperplasia, submucosal venular bleeding; 2: muscle trabeculation, detrusor muscle hypertrophy, bladder diverticula and stone; 3: hydronephrosis and renal failure. B: transurethral resection. The resectoscope is in position. The diathermy cutting loop is drawn back to remove hypertrophied prostate tissue in layers.
Benign prostatic obstruction
Carcinoma of the prostate
Diagnostic plan
FIGURE 9.7b The prostate on rectal examinationA: the normal prostate; B: benign prostatic hypertrophy; C: carcinoma of the prostate
Treatment plan
1 Prostatic obstruction
FIGURE 9.8a Endoscopic view of prostate pre-TURP
FIGURE 9.8b Endoscopic view of prostatic fossa post resection with verum montanum in foreground
2 Urethral stricture
3 Phimosis and meatal stenosis
9.6 Urinary Retention
Causes
Clinical assessment
Diagnostic plan
Treatment plan
FIGURE 9.9 Catheterisation of a distended bladder by percutaneous puncture
9.7 Urinary Incontinence
Types of urinary incontinence
Clinical features
1 Stress incontinence
2 Urge incontinence
3 Continuous or total incontinence
Treatment plan
1 Stress incontinence
2 Urge incontinence
FIGURE 9.10a Fascial sling for stress incontinence
FIGURE 9.10b A retropubic tape such as a TVT and a transobturator tape through the same pelvic bones
Management of complex cases of incontinence
9.8 Penile Lesions
Common causes
Clinical assessment and diagnostic tests
1 Disorders affecting the foreskin
2 Disorders affecting the urethral meatus
3 Disorders affecting the glans
4 Disorders affecting the shaft
5 Sexual and functional disorders
FIGURE 9.11 Peyronie's disease
6 Sexually transmitted infections
Treatment plan
References
Chapter 10 Preoperative medical problems in surgical patients
10.1 Introduction
10.2 Assessing patients for surgery
Box 10.1 A safe system of surgery
FIGURE 10.1 WHO surgical safety checklist
Grading of surgical and anaesthetic risk
TABLE 10.1 ASA classification of anaesthetic risk
Evaluation of the healthy patient
Evaluating elderly asymptomatic patients
Investigations and diagnostic (screening) tests before surgery
Urinalysis
Body weight
Temperature
Full blood examination
Blood typing
Chest x-ray
Electrocardiogram
Preoperative blood transfusion planning
Other tests
10.3 Cardiac disease
Box 10.2 Assessment for surgery: preoperative requirements and tests
All patients
Young, healthy patients (< 60 years), class I surgical risk
Healthy patients 60–70 years, class I surgical risk
Elderly patients > 70 years
Box 10.3 Cardiac risk index: high risk factors
History
Box 10.4 Common perioperative factors that precipitate cardiac decompensation
Box 10.5 Risk factors for ischaemic heart disease
Physical examination
Diagnostic and treatment plan
Non-invasive monitoring
Invasive monitoring
Common cardiac problems
Congestive cardiac failure
Box 10.6 Cardiovascular problems to be controlled before surgery
Ischaemic heart disease (coronary artery disease)
Valvular heart disease
Arrhythmias (and conduction defects)
Hypertension
10.4 Respiratory disease
History and physical examination
Diagnostic plan
Box 10.7 Indications for preoperative lung function tests
Box 10.8 Indicators of critically impaired lung function
Prevention and treatment plan
10.5 Cerebrovascular disease
10.6 Chronic liver disease
Complications arising from chronic liver disease
Box 10.9 Problems associated with alcoholic liver disease
History and physical examination
Diagnostic plan
Box 10.10 Preoperative testing in chronic liver disease
Treatment plan
Box 10.11 Drugs cleared predominantly by the liver
Alcoholic liver disease
10.7 Chronic renal disease
Diagnostic plan
Treatment plan
Box 10.12 Preoperative preparation of patients with chronic renal disease
Box 10.13 Nephrotoxic drugs
Box 10.14 Drugs cleared mainly by the kidney
10.8 Haemostatic and haemopoietic disorders
Box 10.15 Acute renal injury – indications for haemofiltration or dialysis
FIGURE 10.2 Mechanisms of coagulation
Box 10.16 Components of normal haemostasis
Common causes
Clinical assessment
Diagnostic plan
Whole blood clotting time
One-stage prothrombin time
Partial thromboplastin time
Thrombin time
Tests of platelet function
Tests of fibrinolysis
Treatment plan
1 Patients on oral anticoagulants or antiplatelet agents
2 Liver disease
3 Platelet disorders
4 Consumption coagulopathy
TABLE 10.2 Changes during bank storage of whole blood at 4° C after 2 weeks
5 Haemophilia, Christmas disease and Von Willebrand's disease
10.9 Anaemia
Causes of anaemia
Clinical features and diagnostic plan
Treatment plan
10.10 Diabetes mellitus
Diagnostic and treatment plans
Box 10.17 Preoperative management: diabetes mellitus
10.11 Mental health problems
Clinical states
Anxiety disorders
Depressive disorders
Somatoform disorders
Organic mental syndromes
Confusion
Delirium
Dementia
Causes of dementia
Drug dependence and abuse
Diagnostic and treatment plans
Anxiolytics, sedatives and hynotics
Antipsychotics
Antidepressant drugs
10.12 Additional preoperative preparation
Box 10.18a Preoperative preparation: oesophageal surgery
Box 10.18b Preoperative preparation: gastroduodenal surgery
Box 10.19a Preoperative preparation: chronic liver disease
Box 10.19b Preoperative preparation: jaundiced patient
Box 10.20 Preoperative preparation: colorectal surgery
Box 10.21 Preoperative preparation: urological surgery
Box 10.22 Preoperative preparation: vascular surgery
Box 10.23 Preoperative preparation: thyroid surgery
Box 10.24 Preoperative preparation: hernia surgery
Reference
Chapter 11 Postoperative problems
11.1 Introduction
11.2 Pain
TABLE 11.1 Postoperative complications
TABLE 11.2 Commonly used analgesics and dosage guide
11.3 Fever
TABLE 11.3 Causes of postoperative fever
FIGURE 11.1 Causes of fever and onset
11.4 Tachycardia
11.5 Shortness of breath and tachypnoea
Common causes
1 Basal lung atelectasis, bronchitis and bronchopneumonia: ‘the postoperative chest’
FIGURE 11.2 ‘The postoperative chest’A: breathing is impeded centrally and peripherally by wound pain, opiates and anaesthetics; B: ciliary action is depressed by anaesthetics, smoking and chronic bronchitis; C, D: atelectasis results from sputum retention
2 Adult respiratory distress syndrome – acute respiratory failure
Box 11.1 Factors contributing to the development of acute postoperative respiratory failure (adult respiratory distress syndrome)
3 Tension pneumothorax
4 Pulmonary embolism
5 Acute pulmonary oedema
11.6 Low urine output
Common causes
Clinical features and management plan
1 Prerenal – acute vascular insufficiency
TABLE 11.4 Acute renal injury: urine analysis
2 Renal – acute intrinsic renal failure (from acute tubular necrosis)
3 Postrenal – obstructive renal failure
11.7 Sudden collapse or rapid deterioration
TABLE 11.5 Causes of postoperative shock and collapse
Box 11.2 Characteristics of postoperative haemorrhage
Types
Causes
Site of bleeding
11.8 Nausea and vomiting
Box 11.3 Causes of postoperative vomiting
11.9 Confusion and altered mental state
11.10 Wound care problems
Box 11.4 Postoperative wound problems
Early
Late
Box 11.5 Causes of wound dehiscence
Technical error
Local factors
General factors
11.11 Abnormal investigations
Hypokalaemia
Hyperkalaemia
Hydrogen ion (acid–base) disorders
TABLE 11.6 Changes in arterial blood chemistry with hydrogen ion disturbances
Metabolic acidosis
Metabolic alkalosis
Respiratory acidosis and alkalosis
Chapter 12 Problems in surgical intensive care
12.1 Introduction: What is intensive care?
12.2 Patient selection
Post elective surgery
Post emergency surgery
Unplanned admission from the surgical ward
Scoring systems
12.3 Throughput and efficiency
12.4 ICU versus high dependency unit care
12.5 Postoperative ICU care
Monitoring – an overview
Invasive monitoring
Intra-arterial blood pressure monitoring
Central venous access and monitoring
TABLE 12.1 Examples of monitoring by systems
FIGURE 12.1 Swan-Ganz catheterA: line to inflate the balloon in pulmonary microvasculature; B: lumen for measuring pulmonary artery pressure/pulmonary capillary wedge pressure; C: lumen for measuring right atrial pressure (central venous pressure); D: thermistor catheter for measuring cardiac output by thermodilution
FIGURE 12.2 Radial artery cannulation
Pulmonary artery (Swan-Ganz) catheters
FIGURE 12.3 Central venous catherisationA: infraclavicular (subclavian) approach; B: internal jugular approach
Non-invasive monitoring
Nursing care
Organ preservation
Wound healing in the ICU
Pain management
Nutrition
Enteral feeding
FIGURE 12.4 Percutaneous jejunostomy
Parenteral feeding or total parenteral nutrition
FIGURE 12.5 Hickman catheterA: a silicone catheter is inserted into the right atrium via the cephalic vein: B: subcutaneous tunnel; C: a Teflon cuff reduces ascending infection and prevents inadvertent removal
12.6 Recovery and discharge from the ICU to the surgical ward
FIGURE 12.6 Parenteral nutritionA: TPN/balanced nutrient solution; B: monitoring pump; C: Hickman catheter; D: bag for collection of fistula loss; E: urinary catheter; F: blood collection for routine measurement of Na, K, Cl, PO4, HCO3, glucose, urea, creatinine, albumin and osmolality
12.7 General management of ICU patients
12.8 Cardiopulmonary arrest
12.9 Common problems in the ICU
Fever
Systemic inflammatory response syndrome
Sepsis
TABLE 12.2 Criteria for systemic inflammatory response syndrome
Hypoxia and hypercarbia
Hypotension and shock
TABLE 12.3 Causes of hypotension and shock, by group
Inotropes and vasopressors
Hypertension
Metabolic and electrolyte disturbances
Acid–base disorders
Metabolic acidosis
Metabolic alkalosis
Respiratory acidosis
TABLE 12.4 Definitions of acidaemia and alkalaemia
TABLE 12.5 Causes of metabolic acidosis
Respiratory alkalosis
Other metabolic disorders
Electrolyte disorders
Sodium and water (disorders of tonicity)
Hyponatremia
Hypernatremia
Disorders of potassium
TABLE 12.6 Example causes of potassium imbalance
Magnesium
Oliguria/renal dysfunction and renal replacement
Box 12.1 Causes of renal dysfunction/oliguria in the ICU
Hepatic and gastrointestinal dysfunction
Neurological dysfunction
Box 12.2 Central causes of neurological dysfunction
Peripheral causes
Haematological dysfunction and haemorrhage
Massive haemorrhage
Multiple organ dysfunction syndrome (MODS)
12.10 The dying patient
12.11 Limitation of treatment/not for escalation of care orders
12.12 Withdrawal of treatment
12.13 Brain death and organ and tissue donation
Brain death
Organ and tissue donation
References
Chapter 13 Problems in injured patients
13.1 Introduction
Box 13.1 The ‘DRABC’ first aid action plan
13.2 Managing injured patients
Initial assessment
Primary survey and resuscitation
A Airway and cervical spine
TABLE 13.1 Important investigations and procedures following the primary survey and resuscitation
FIGURE 13.1a In the unconscious patient the tongue falls back
B Breathing and ventilation
FIGURE 13.1b Head tilt, chin lift and jaw thrust manoeuvres
FIGURE 13.2a Adequate airwayIn the unconscious patient the airway is first cleared by making sure that the tongue is forward and that the pharynx is clear of foreign bodies.
FIGURE 13.2b Endotracheal intubation: passage of an endotracheal tubeNasotracheal intubation is preferable when there is a danger of cervical spine injury.
Oxygenation
FIGURE 13.2c Nasopharyngeal airway with bag-valve mask and reservoir device
TABLE 13.2 Summary of airway management
C Circulation and control of haemorrhage
FIGURE 13.2d Oropharyngeal airway with bag-valve mask
TABLE 13.3 Recognition and initial management of life-threatening thoracic injuries
Fluid resuscitation
FIGURE 13.3 Venous cutdownA: incision above and anterior to the medial malleolus; B: the vein margins are defined; C: a length of vein is cleared; D: the vein is elevated and ligated; E: a bevelled incision is made and the vein is cannulated; F: the catheter is tied in and infusion begins
D Disability and neurological assessment
E Exposure and environmental control
Diagnostic peritoneal lavage
Secondary survey
History
Box 13.2 Useful questions to ask an ambulance officer at handover (e.g. for motor vehicle accident)
Examination
Neurological: Glasgow coma scale
Investigations and procedures following the secondary survey
Re-evaluation
Pain relief and splinting
Definitive care and transfer
Interhospital transfer
Medical records and documentation
Shock
FIGURE 13.4 Example of medical record/documentation
Clinical features of haemorrhagic shock
Diagnostic and treatment plan
13.3 Soft tissue injury and wound care
Classification of wounds
1 Clean wounds
2 Clean–contaminated wounds
TABLE 13.4 Classification of wounds
3 Contaminated wounds
4 Dirty–infected wounds
Principles of wound healing
Phases in wound healing
Factors adversely affecting wound healing
Local factors
General factors
Box 13.3 Local factors that interfere with wound healing
Box 13.4 General or host factors that interfere with wound healing
Definitive care
Wound care – debridement
Wound closure
Timing of wound closure
Wound closure techniques and materials
FIGURE 13.5 Local wound flapsIn random flaps without an axial blood supply the ratio of length to width should not exceed 1 : 1.
FIGURE 13.6 Local flaps: Z-plasty flap
Closed soft tissue (sporting) injuries
FIGURE 13.7 TRAM flap used for reconstruction after mastectomy
13.4 Burns
History
Types
Pathophysiology of burns
Local response to burns: Jackson's burn zones
Systemic response to burns: SIRS and MODS
First aid
FIGURE 13.8 Jackson's burn zones
Initial assessment
Extent of burns
FIGURE 13.9 ‘Rule of nines’ – calculating the percentage distribution of burnt skin in an adult and childA: adult burns chart B: paediatric burns chart
Classification of burn depth
Assessment of burn depth
FIGURE 13.10 Depth of burnsA: full-thickness (deep) burn; B: partial-thickness (superficial) burn
Burns to the respiratory tract
Subsequent assessment and definitive care
General management
Monitoring
Burn wound management
Box 13.5 Patients who fulfill the following criteria should be considered for transfer to a specialist burns unit
FIGURE 13.11 Locations for escharotomiesThe incisions are placed along the midmedial and midlateral lines of the extremities and the thorax (dashed lines). The skin is especially tight along major joints, and decompression at these sites must be complete (solid lines). Neck and digital escharotomies are rarely necessary.
13.5 Head injury
Classification and definitions
Primary injury: focal lesions
FIGURE 13.12a Mechanism of contrecoup injury
FIGURE 13.12b Coronal section of a patient undergoing herniations of the brain caused by an EDHA and B based on Williamson & Waxman 1998
Primary injury: diffuse lesions
Secondary injury
Initial assessment
Primary survey and resuscitation
Secondary survey
Examination of the scalp and face
Abnormal neurological signs
History
Re-evaluation
Investigations
Plain x-ray
TABLE 13.5 Head injury: testing of cranial nerve function after head injury
FIGURE 13.13 Conscious state and head injury chart
FIGURE 13.14 Guide to recording neurological observation chart
CT scan
Lumbar puncture
Magnetic resonance imaging
Cerebral angiography
Definitive care
General principles of management
Management of mild head injury (GCS 14–15)
Management of moderate head injury (GCS 9–13)
Management of severe head injury (GCS 3–8)
Management of specific complications
Box 13.6 Complications of head injury
FIGURE 13.15 Complications of basal skull fractureA: anterior fossa fracture with posterior conjunctival haemorrhage, CSF rhinorrhoea and epistaxis; B: middle fossa fractures with bleeding and CSF leak from the ear
13.6 Facial injury
Initial assessment
TABLE 13.6 Zonal classification of facial skeletal injuries
Le Fort classification
FIGURE 13.16 Blowout fracture of the orbital floor with an intact orbital rimThe entrapped inferior rectus muscle produces diplopia on upward gaze.
Mandibular fractures
Adjuncts to initial assessment
Definitive care
FIGURE 13.17 Le Fort classification of fractures of the maxillaI: the infraorbital rim remains stable as the maxilla is rocked; II: only the medial section of the infraorbital rim moves – associated infraorbital nerve damage is common; III: the whole of the infraorbital rim moves with the maxilla
13.7 Eye and orbital injury
Introduction
History taking
Examination
Chemical injury
First aid
Clinical assessment
Treatment plan
Corneal flash burns
Clinical assessment
Treatment plan
Perforating globe injuries
Clinical assessment
FIGURE 13.18 Anatomy of the globe
First aid
Diagnostic plan
Treatment plan
Superficial foreign body injury
Clinical assessment
Treatment plan
Closed globe injury
Clinical assessment
Diagnostic plan
Treatment plan
Injury to the orbit
Clinical assessment
FIGURE 13.19 Anatomy of the orbit
Diagnostic plan
Treatment plan
Injury to the eyelids
FIGURE 13.20 Anatomy of the lacrimal system
Clinical assessment
Treatment plan
13.8 Chest injury
Initial assessment
Primary survey
Secondary survey
Investigations
Definitive care
General management
Insertion of an intercostal catheter
Management of specific types of chest injury
FIGURE 13.21 Tube thoracotomyA: the fourth intercostal space is exposed in the midaxillary line; B: a tunnel is made with an artery forcep starting over the fifth rib and directed under the fourth rib; C: finger or artery forceps entry is made into the pleural space; D: a large tube is inserted in a posterosuperior direction and sutured to the skin; E: the intercostal tube is attached to underwater drainage
13.9 Abdominal injury
Blunt trauma
Box 13.7 Principles of surgical management of abdominal injury
Penetrating trauma
Initial assessment
Investigations
FIGURE 13.22 Blunt abdominal traumaCommon sites of injury – 1: liver; 2: pancreas; 3: duodenum; 4: spleen; 5: small bowel and mesentery; 6: caecum; 7: urinary bladder
Diagnostic modalities available for intra-abdominal trauma
FIGURE 13.23 Diagnostic peritoneal lavage in blunt trauma
Definitive care
Laparotomy and damage control principles
Damage control laparotomy
Abdominal compartment syndrome
Management of specific organ injuries
TABLE 13.7 The AAST splenic organ injury scaling system, 1994 revision
13.10 Nerve injury
FIGURE 13.24 Extraperitoneal injuries of the rectumA: defunctioning sigmoid colostomy; B: intraperitoneal drain; C: repair of rectal wound; D: extraperitoneal presacral drain
Classification
FIGURE 13.25 Peripheral nerve injuries1: endoneurium; 2: axon; 3: myelin. Peripheral nerve injuryA: neurapraxia; B: axonotmesis: axonal regrowth occurs at 1 mm per day; C: neurotmesis: a neuroma forms unless the axon has become connected with the distal sheath by suturing
Initial assessment
Sensory assessment
FIGURE 13.26 Common closed peripheral nerve injuries1: circumflex (axillary) nerve with deltoid paralysis and sensory loss; 2: radial nerve with wrist and finger drop and minor sensory loss; 3: ulnar nerve with sensory loss and inability to abduct the minimus; 4: median nerve with sensory loss and loss of palmar abduction of pollex; 5: sciatic nerve with foot drop, extensive sensory loss and loss of ankle jerk; 6: lateral popliteal (common peroneal) nerve with sensory loss and foot drop
Motor assessment
Definitive care
Open wounds with nerve injury
Autonomic dysfunction after injury – vasomotor dystrophy
13.11 Vascular injury
Classification
Initial assessment
Box 13.8 Common blunt injuries leading to closed vascular injury
Box 13.9 Major signs of vascular injury
Investigations
Definitive care
General principles
Principles of surgical management
FIGURE 13.27 Vascular repairA: end-to-end anastomosis; B: vein graft; C: synthetic graft; D: lateral suture with or without endarterectomy; E: patch angioplasty
Management of specific vascular injuries
FIGURE 13.28 Fasciotomy of the lower limbTwo skin incisions (A and B) are sufficient to decompress the anterior, lateral and posterior compartments (1, 2 and 3).
Box 13.10 Indications for fasciotomy
Box 13.11 Specific vascular injuries
FIGURE 13.29 Anatomical zones of the neck
Box 13.12 Reasons for failure of repair of a vascular injury
Box 13.13 Precautions to avoid inadvertent arterial injection
13.12 Urinary tract injury
Renal injury
Initial assessment
TABLE 13.8 AAST organ injury severity scale (1989) for the kidney
Definitive care
Surgical intervention
Conservative management
Ureteral injury
Bladder and urethral injury
Initial assessment
Bladder and posterior urethral injuries
Bladder injuries
Posterior (prostatomembranous) urethral rupture
FIGURE 13.30 Extraperitoneal rupture of the bladder or posterior (prostatomembranous) urethraUrinary extravasation above the urogenital diaphragm.A: shearing strain when the pelvic ring is broken and displaced; B: on rectal examination a haematoma obscures the prostate
Injuries to the anterior urethra
Investigations
Definitive care
In patients with suspected anterior urethral injuries
In patients with suspected posterior urethral or bladder injury
Posterior urethral injury
Bladder injury
13.13 Spinal injury
Classification of spinal cord injury
Neurological patterns of injury
FIGURE 13.31 Spinal cord injury: levels of function
Initial assessment
Primary survey
Secondary survey
Investigations
Definitive care
Management in an emergency department
Transfer to a spinal unit
13.14 Major fractures and joint injury
Initial assessment
Primary survey
Resuscitation
Secondary survey
Investigations
Definitive care
Principles of management
Methods of management
FIGURE 13.32 External fixation to facilitate soft tissue repairExternal fixation stabilises an open comminuted fracture of the tibia associated with extensive tissue damage, and facilitates soft tissue repair.
Compartment syndrome
Rhabdomyolysis and renal impairment
13.15 Hand injury
Initial assessment
Assessing the hand
Investigations
Definitive care
Principles of surgical management
Digital reimplantation and microsurgery
Wound closure
Postoperative management and secondary procedures
Chapter 14 Ophthalmological problems
14.1 Introduction
14.2 Who's who in eye care
Ophthalmologist
Optometrist
Orthoptist
14.3 Basic anatomy of the eye
14.4 Ocular symptoms
FIGURE 14.1 Basic anatomy of the eye
Box 14.1 Relevance of ophthalmology in general medicine and surgery
14.5 The basic eye examination
Visual acuity
TABLE 14.1 Clustering of ophthalmic symptoms
Distance visual acuity testing and recording
FIGURE 14.2 Occlusion with palm
FIGURE 14.3 Standard Snellen visual acuity chart, C chart and E chartThe patient should be encouraged to read the smaller letters or the next line even if they are not confident of the letters.
Pupils
Visual fields
FIGURE 14.4 Normal pupils
FIGURE 14.5 Relative afferent pupil defect (RAPD)
FIGURE 14.6 Confrontation field testing
Eye movements
Gross examination of the eye and adnexae
Eyelids and surrounding tissue
TABLE 14.2 Cardinal position of gaze, extraocular muscles and their cranial nerve supply
FIGURE 14.7 Eye movement testing
Gross inspection of the eye
Additional tests
Direct ophthalmoscope
Operating a direct ophthalmoscope
Clinical examination using a direct ophthalmoscope
FIGURE 14.8 The direct ophthalmoscope
Slit lamp examination of the eye and adnexae
FIGURE 14.9 Normal (A) and swollen (B) optic nerve appearance
14.6 Diagnosis of common problems
Loss of vision
Differential diagnosis
Acute loss of vision
Transient visual loss
Persistent visual loss lasting more than 24 hours
Gradual painless loss of vision
Binocular visual loss
History
Duration of symptoms
Associated symptoms
Previous ophthalmic history
Previous medical history including drug history
Family history
Social history
Examination
Visual acuity
Pupils
Visual fields
FIGURE 14.10 Localised corneal opacity secondary to infective microbial keratitis
Eye movements
Anterior segment examination
FIGURE 14.11 Diffuse corneal oedema due to congenital glaucoma
FIGURE 14.12 Corneal dendritic ulcer
FIGURE 14.13 HypopyonA hypopyon is the settling of inflammatory cells in the anterior chamber due to severe inflammation caused by infective or non-infective sight-threatening conditions.
FIGURE 14.14 HyphaemaA hypahema is the settling of red blood cells in the anterior chamber usually secondary to blunt trauma of the eye.
Fundoscopy
Primary management
Ongoing management
14.7 Double vision – ‘diplopia’
Monocular diplopia
Differential diagnosis
Binocular diplopia
Differential diagnosis
History
Nature of the double vision
Associated symptoms
Examination
Visual acuity with pinhole
Pupil examination
Inspection
Cover test
Eye movements
Cranial nerve examination
Primary management
Neuroimaging
Bloods
Ongoing management
14.8 Red or painful eye
History
Duration of symptoms
TABLE 14.3 Common systemic causes of red eye
Description of pain
Associated symptoms
Previous ophthalmic history
Previous medical history
Primary management
TABLE 14.4 Common differential diagnosis for a red painful eye
14.9 Common lumps and bumps around the eye
Eyelid swelling
Causes
14.10 Selected ophthalmic conditions
Preseptal and orbital cellulitis
Preseptal cellulitis
Aetiology
Signs
Treatment
1 Outpatient treatment
2 Inpatient treatment
Orbital cellulitis
Aetiology
TABLE 14.5 Common eyelid lumps and bumps
Symptoms and signs
Complications
Ocular
TABLE 14.6 Preseptal vs orbital cellulitis
TABLE 14.7 Causes of orbital cellulitis
Systemic
Investigations
Treatment
Microbial keratitis
Common bacterial pathogens
Clinical features
Symptoms
Signs
TABLE 14.8 Common predisposing factors
Differential diagnosis
Investigations
Treatment
Indications for hospital admission
Conjunctivitis
Adenoviruses
Symptoms
Signs
FIGURE 14.15 Conjunctival follicles – discrete, yellowish, slightly elevated lesions most prominent in the fornices
FIGURE 14.16 Conjunctival membrane secondary to viral conjunctivitis
Investigations
Management
Bacterial conjunctivitis in neonates: ophthalmia neonatorum
Aetiology
Signs
Systemic complications
Investigations
FIGURE 14.17 Purulent conjunctival discharge
Treatment
Lens and cataract
Symptoms
Signs
Treatment
FIGURE 14.18 Modern phacoemulsification cataract surgery
Acute angle closure
Risk factors
Symptoms
Signs
Complications of high IOP
Treatment
Emergency treatment and refer to an ophthalmologist
Definitive treatment
Diabetic retinopathy
Non-proliferative diabetic retinopathy
Proliferative diabetic retinopathy
Symptoms
Signs
Treatment
Systemic
Ophthalmic
Uveitis
Symptoms
Signs
Investigations
FIGURE 14.19 a. Posterior synechia (arrow) in a partially dilated pupil
b. Cells and flare in the anterior chamber on slit lamp examination
Treatment
Retinal detachment
Risk factors
Symptoms
Giant cell arteritis
Symptoms
Ophthalmic
Systemic
Signs
Ophthalmic
Systemic
Investigations
Systemic
Ophthalmic
Referral
Initial treatment
Prophylactic treatment
Temporal artery biopsy
Further treatment and follow up
Natural history
Principles of treatment
Visual prognosis
Ischaemic cranial nerve palsies: third, fourth and sixth
History
Examination
On follow-up
Ischaemic third nerve palsy
Specific history
Motility examination
Ischaemic fourth nerve palsy
Specific history
Motility examination
Ischaemic sixth nerve palsy
Specific history
Motility examination
Paediatric ophthalmology
Amblyopia
Abnormal red-reflex
FIGURE 14.20 A. Normal red reflex
B. Leucocoria due to retinoblastoma
Retinoblastoma
History
Investigations
FIGURE 14.21 Right eye retinoblastoma
Treatment
Reference
Picture Credits
Chapter 1
Chapter 2
Chapter 3
Chapter 4
Chapter 6
Chapter 7
Chapter 9
Chapter 10
Chapter 13
Chapter 14
| An aparitie | 06-Apr-17 |
| Autor | Julian A. Smith MBBS MS MSurgEd FRACS FACS FFSTRCSEd FCSANZ FAICD , Jane G. Fox MBBS FRACS |
| Dimensiuni | 19.05 x 2.54 x 25.4 cm |
| Editura | Elsevier |
| Format | Paperback |
| ISBN | 9780729542265 |
| Limba | Engleza |
| Nr pag | 560 |

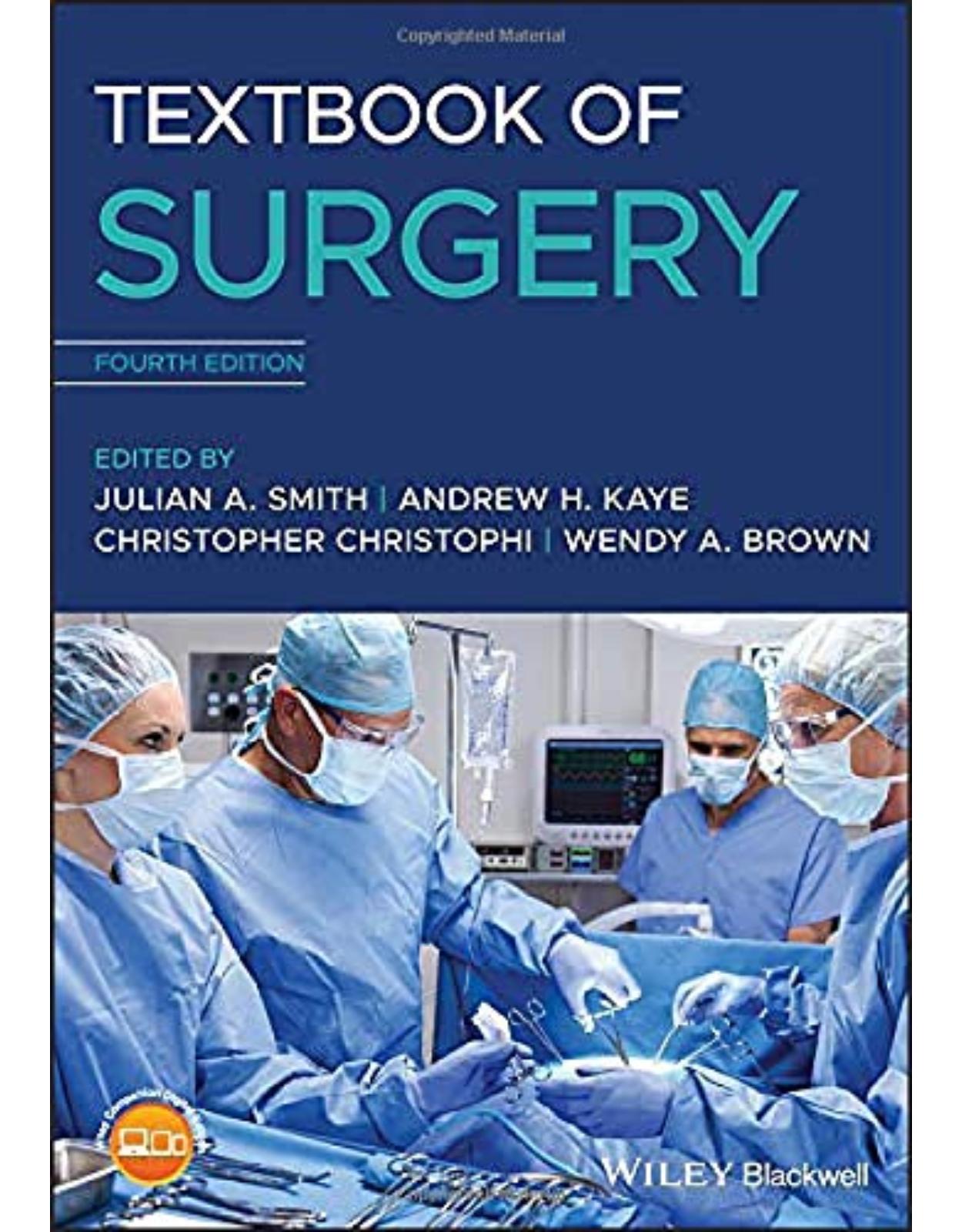
Clientii ebookshop.ro nu au adaugat inca opinii pentru acest produs. Fii primul care adauga o parere, folosind formularul de mai jos.