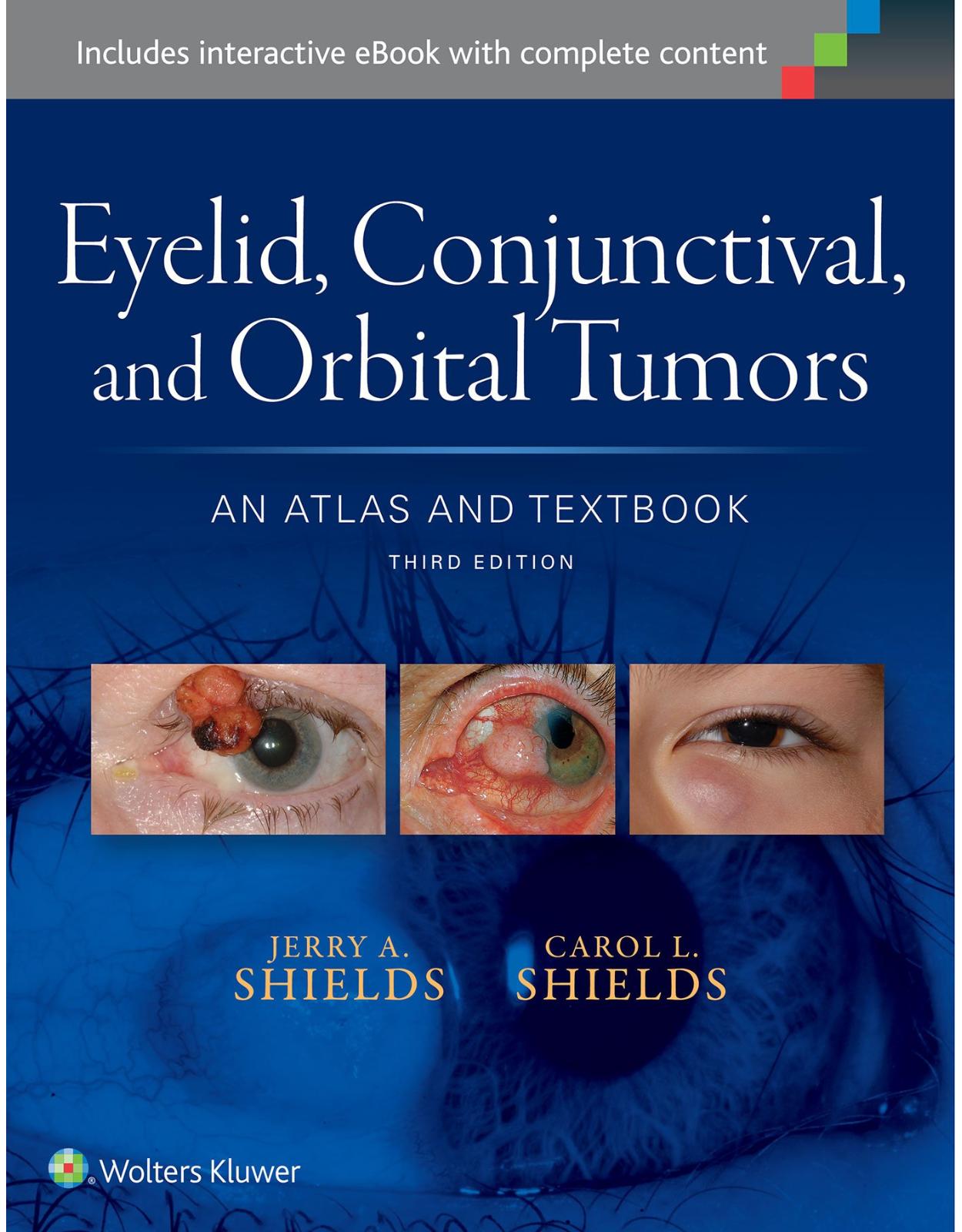
Eyelid, Conjunctival, and Orbital Tumors: An Atlas and Textbook
Livrare gratis la comenzi peste 500 RON. Pentru celelalte comenzi livrarea este 20 RON.
Disponibilitate: La comanda in aproximativ 4-6 saptamani
Editura: LWW
Limba: Engleza
Nr. pagini: 824
Coperta: Hardcover
Dimensiuni: 213 x 276 x 40 mm
An aparitie: 17 Oct. 2015
Description:
For outstanding visual clarity in ocular diagnosis … nothing else comes close.In this updated and revised third edition, world-renowned authorities from the Wills Eye Hospital provide outstanding guidance on recognition, evaluation, and treatment of ocular tumors, highlighted by more than 3,000 stunning photographs and surgical drawings. This unsurpassed ocular oncology resource is a comprehensive guide to the clinical features, diagnosis, management, and pathology of eyelid, conjunctival, and orbital tumors and pseudotumors, depicting clinical variations, treatment and histopathologic characteristics of the wide spectrum of neoplasms and related lesions. Now brought thoroughly up to date with recent clinical and scientific innovations, this unique volume offers more high-quality images than any other text/atlas in the field.Presents each entity in an easy-to-follow format: a concise description with references on the left-hand page and six illustrations on the right-hand page.Depicts in precise photographic detail the gross and microscopic features that distinguish each type of lesion, while professional drawings and intraoperative photographs demonstrate key surgical principles and procedures.Includes numerous new references regarding diagnosis and treatment, as well as new scientific tables containing key information for your clinical practice.Features 25% new images, including panoramic images, surgical images, diagnostic testing images from multiple modalities, and updated, high resolution MRI and CT scans.Covers new information on evolving conditions such as IgG4 orbital inflammatory disease, solitary fibrous tumor of the orbit, and lymphoid proliferations of the orbit, conjunctiva, and globe; as well as new methods of nonsurgical therapy such as topical chemotherapy, intravenous chemotherapy, and immunotherapy and biological therapy with Rituxan for lymphoma; and new information on classification of various tumors and expected outcomes are clearly displayed in table format.Now with the print edition, enjoy the bundled interactive eBook edition, which can be downloaded to your tablet and smartphone or accessed online and includes features like:Complete content with enhanced navigationPowerful search tools and smart navigation cross-links that pull results from content in the book, your notes, and even the webCross-linked pages, references, and more for easy navigationHighlighting tool for easier reference of key content throughout the textAbility to take and share notes with friends and colleaguesQuick reference tabbing to save your favorite content for future use
Table of Contents:
Part 1: Tumors of the Eyelids
Chapter 1: Benign Tumors of the Eyelid Epidermis
Eyelid Squamous Papilloma
General Considerations
Clinical Features
Differential Diagnosis
Pathology
Management
Prognosis
Selected References
Eyelid Squamous Papilloma
Figure 1.1
Figure 1.2
Figure 1.3
Figure 1.4
Figure 1.5
Figure 1.6
Eyelid Seborrheic Keratosis
General Considerations
Clinical Features
Differential Diagnosis
Pathology and Pathogenesis
Management
Prognosis
Selected References
Eyelid Seborrheic Keratosis
Figure 1.7
Figure 1.8
Figure 1.9
Figure 1.10
Figure 1.11
Figure 1.12
Eyelid Seborrheic Keratosis: Clinical Variations
Figure 1.13
Figure 1.14
Figure 1.15
Figure 1.16
Figure 1.17
Figure 1.18
Eyelid Inverted Follicular Keratosis
General Considerations
Clinical Features
Differential Diagnosis
Pathology
Management
Prognosis
Selected References
Eyelid Inverted Follicular Keratosis
Figure 1.19
Figure 1.20
Figure 1.21
Figure 1.22
Figure 1.23
Figure 1.24
Eyelid Pseudoepitheliomatous Hyperplasia
General Considerations
Clinical Features
Differential Diagnosis
Pathology
Management
Selected References
Eyelid Pseudoepitheliomatous Hyperplasia
Figure 1.25
Figure 1.26
Figure 1.27
Figure 1.28
Figure 1.29
Figure 1.30
Eyelid Keratoacanthoma and Nonspecific Keratosis
General Considerations
Clinical Features
Differential Diagnosis
Pathology and Pathogenesis
Management
Nonspecific Keratosis
Selected References
Eyelid Keratoacanthoma
Figure 1.31
Figure 1.32
Figure 1.33
Figure 1.34
Figure 1.35
Figure 1.36
Eyelid Keratoacanthoma: Case Description and Management by Excision and Skin Graft
Figure 1.37
Figure 1.38
Figure 1.39
Figure 1.40
Figure 1.41
Figure 1.42
Eyelid Keratoacanthoma: Clinicopathologic Correlation in Young and Elderly Patients
Figure 1.43
Figure 1.44
Figure 1.45
Figure 1.46
Figure 1.47
Figure 1.48
Eyelid Nonspecific Keratosis
Figure 1.49
Figure 1.50
Figure 1.51
Figure 1.52
Figure 1.53
Figure 1.54
Chapter 2: Premalignant and Malignant Tumors of Eyelid Epidermis
Eyelid Actinic Keratosis
General Considerations
Clinical Features
Differential Diagnosis
Pathology and Pathogenesis
Management
Prognosis
Selected References
Eyelid Actinic Keratosis
Figure 2.1
Figure 2.2
Figure 2.3
Figure 2.4
Figure 2.5
Figure 2.6
Cutaneous Actinic Keratosis: Association with Conjunctival Squamous Cell Carcinoma
Figure 2.7
Figure 2.8
Figure 2.9
Figure 2.10
Figure 2.11
Figure 2.12
Radiation Blepharopathy
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Eyelid Radiation Blepharopathy
Figure 2.13
Figure 2.14
Figure 2.15
Figure 2.16
Figure 2.17
Figure 2.18
Eyelid Xeroderma Pigmentosum
General Considerations
Clinical Features
Diagnosis
Pathology
Management
Selected References
Eyelid Xeroderma Pigmentosum
Figure 2.19
Figure 2.20
Figure 2.21
Figure 2.22
Figure 2.23
Figure 2.24
Sebaceous Nevus
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Eyelid Sebaceous Nevus: Association with Periocular Involvement
Figure 2.25
Figure 2.26
Figure 2.27
Figure 2.28
Figure 2.29
Figure 2.30
Eyelid Basal Cell Carcinoma
General Considerations
Clinical Features
Differential Diagnosis
Pathology
Pathogenesis
Management
Nevoid Basal Cell Carcinoma Syndrome
Selected References
Eyelid Basal Cell Carcinoma: Nodular and Noduloulcerative Type
Figure 2.31
Figure 2.32
Figure 2.33
Figure 2.34
Figure 2.35
Figure 2.36
Eyelid Basal Cell Carcinoma: Morpheaform (Sclerosing) Type
Figure 2.37
Figure 2.38
Figure 2.39
Figure 2.40
Figure 2.41
Figure 2.42
Eyelid Basal Cell Carcinoma: Clinical Variations
Figure 2.43
Figure 2.44
Figure 2.45
Figure 2.46
Figure 2.47
Figure 2.48
Eyelid Basal Cell Carcinoma: Advanced Cases
Figure 2.49
Figure 2.50
Figure 2.51
Figure 2.52
Figure 2.53
Figure 2.54
Eyelid Basal Cell Carcinoma: Nevoid Basal Cell Carcinoma Syndrome (Gorlin–Goltz Syndrome)
Figure 2.55
Figure 2.56
Figure 2.57
Figure 2.58
Figure 2.59
Figure 2.60
Eyelid Basal Cell Carcinoma: Nevoid Basal Cell Carcinoma Syndrome (Gorlin–Goltz Syndrome) with Multiple Cutaneous Malignancies
Figure 2.61
Figure 2.62
Figure 2.63
Figure 2.64
Figure 2.65
Figure 2.66
Eyelid Basal Cell Carcinoma: Nevoid Basal Cell Carcinoma Syndrome (Gorlin–Goltz Syndrome) with Odontogenic Keratocyst
Figure 2.67
Figure 2.68
Figure 2.69
Figure 2.70
Figure 2.71
Figure 2.72
Eyelid Basal Cell Carcinoma: Management with Pentagonal Full-Thickness Eyelid Resection and Topical Imiquimod
Figure 2.73
Figure 2.74
Figure 2.75
Figure 2.76
Figure 2.77
Figure 2.78
Eyelid Basal Cell Carcinoma: Results of Surgical Management
Figure 2.79
Figure 2.80
Figure 2.81
Figure 2.82
Figure 2.83
Figure 2.84
Eyelid Basal Cell Carcinoma: Advanced, Neglected Cases Managed by Orbital Exenteration
Figure 2.85
Figure 2.86
Figure 2.87
Figure 2.88
Figure 2.89
Figure 2.90
Eyelid Squamous Cell Carcinoma
General Considerations
Clinical Features
Differential Diagnosis
Pathology
Pathogenesis
Management
Prognosis
Selected References
Eyelid Squamous Cell Carcinoma
Figure 2.91
Figure 2.92
Figure 2.93
Figure 2.94
Figure 2.95
Figure 2.96
Eyelid Squamous Cell Carcinoma: Diffuse Involvement of Upper Eyelid
Figure 2.97
Figure 2.98
Figure 2.99
Figure 2.100
Figure 2.101
Figure 2.102
Eyelid Squamous Cell Carcinoma: Aggressive Invasive Tumors
Figure 2.103
Figure 2.104
Figure 2.105
Figure 2.106
Figure 2.107
Figure 2.108
Eyelid Squamous Cell Carcinoma: Deep Cystic Recurrent Tumor
Figure 2.109
Figure 2.110
Figure 2.111
Figure 2.112
Figure 2.113
Figure 2.114
Chapter 3: Eyelid Sebaceous Gland Tumors
Eyelid Sebaceous Hyperplasia and Adenoma
General Considerations
Muir–Torre Syndrome
Clinical Features
Pathology
Management
Selected References
Eyelid Sebaceous Carcinoma
General Considerations
Clinical Features
Classification
Differential Diagnosis
Pathology
Management
Prognosis
Selected References
Table 3.1: American Joint Committee on Cancer (AJCC) classification of periocular sebaceous gland carcinoma
Eyelid Sebaceous Carcinoma: Meibomian Gland Origin
Figure 3.1
Figure 3.2
Figure 3.3
Figure 3.4
Figure 3.5
Figure 3.6
Eyelid Sebaceous Carcinoma: Zeis Gland Origin
Figure 3.7
Figure 3.8
Figure 3.9
Figure 3.10
Figure 3.11
Figure 3.12
Eyelid Sebaceous Carcinoma: Diffuse Neoplasm Masquerading as Inflammation
Figure 3.13
Figure 3.14
Figure 3.15
Figure 3.16
Figure 3.17
Figure 3.18
Eyelid Sebaceous Carcinoma: Pedunculated Variant
Figure 3.19
Figure 3.20
Figure 3.21
Figure 3.22
Figure 3.23
Figure 3.24
Eyelid Sebaceous Carcinoma: Clinical Variations and Histopathology
Figure 3.25
Figure 3.26
Figure 3.27
Figure 3.28
Figure 3.29
Figure 3.30
Eyelid Sebaceous Tumors: Association with Muir–Torre Syndrome
Figure 3.31
Figure 3.32
Figure 3.33
Figure 3.34
Figure 3.35
Figure 3.36
Eyelid Sebaceous Carcinoma: Diffuse Neoplasm
Figure 3.37
Figure 3.38
Figure 3.39
Figure 3.40
Figure 3.41
Figure 3.42
Eyelid Sebaceous Carcinoma: Aggressive Clinical Course
Figure 3.43
Figure 3.44
Figure 3.45
Figure 3.46
Figure 3.47
Figure 3.48
Eyelid Sebaceous Carcinoma: Pentagonal Full-Thickness Eyelid Resection
Figure 3.49
Figure 3.50
Figure 3.51
Figure 3.52
Figure 3.53
Figure 3.54
Eyelid Sebaceous Carcinoma: Pentagonal Resection and Semicircular Flap Reconstruction
Figure 3.55
Figure 3.56
Figure 3.57
Figure 3.58
Figure 3.59
Figure 3.60
Eyelid Sebaceous Carcinoma: Large Tumor and Rotational Forehead Flap
Figure 3.61
Figure 3.62
Figure 3.63
Figure 3.64
Figure 3.65
Figure 3.66
Eyelid Sebaceous Carcinoma: Posterior Lamellar Eyelid Resection and Reconstruction
Figure 3.67
Figure 3.68
Figure 3.69
Figure 3.70
Figure 3.71
Figure 3.72
Chapter 4: Eyelid Sweat Gland Tumors
Eyelid Syringoma
General Considerations
Clinical Features
Differential Diagnosis
Pathology
Management
Selected References
Eyelid Syringoma
Figure 4.1
Figure 4.2
Figure 4.3
Figure 4.4
Figure 4.5
Figure 4.6
Eyelid Eccrine Acrospiroma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eccrine Acrospiroma
Figure 4.7
Figure 4.8
Figure 4.9
Figure 4.10
Figure 4.11
Figure 4.12
Eyelid Syringocystadenoma Papilliferum
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Syringocystadenoma Papilliferum
Figure 4.13
Figure 4.14
Figure 4.15
Figure 4.16
Figure 4.17
Figure 4.18
Eyelid Pleomorphic Adenoma (Benign Mixed Tumor)
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Pleomorphic Adenoma (Benign Mixed Tumor)
Figure 4.19
Figure 4.20
Figure 4.21
Figure 4.22
Figure 4.23
Figure 4.24
Eyelid Sweat Gland Adenocarcinoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Mucinous Sweat Gland Adenocarcinoma
Figure 4.25
Figure 4.26
Figure 4.27
Figure 4.28
Figure 4.29
Figure 4.30
Eyelid Sweat Gland Carcinoma
Figure 4.31
Figure 4.32
Figure 4.33
Figure 4.34
Figure 4.35
Figure 4.36
Chapter 5: Eyelid Hair Follicle Tumors
Eyelid Trichoepithelioma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid and Facial Trichoepithelioma
Figure 5.1
Figure 5.2
Figure 5.3
Figure 5.4
Figure 5.5
Figure 5.6
Eyelid Trichofolliculoma and Trichoadenoma
General Considerations
Clinical Features
Pathology
Management
Trichoadenoma
Selected References
Eyelid Trichofolliculoma and Trichoadenoma
Figure 5.7
Figure 5.8
Figure 5.9
Figure 5.10
Figure 5.11
Figure 5.12
Eyelid Trichilemmoma
General Considerations
Clinical Features
Cowden’s Disease
Pathology
Management
Selected References
Eyelid Trichilemmoma, Trichilemmal Carcinoma, and Cowden’s Syndrome
Figure 5.13
Figure 5.14
Figure 5.15
Figure 5.16
Figure 5.17
Figure 5.18
Eyelid Pilomatrixoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Pilomatrixoma in Adults
Figure 5.19
Figure 5.20
Figure 5.21
Figure 5.22
Figure 5.23
Figure 5.24
Eyelid Pilomatrixoma in Children: Surgical Excision
Figure 5.25
Figure 5.26
Figure 5.27
Figure 5.28
Figure 5.29
Figure 5.30
Eyelid Pilomatrixoma: Surgical Excision and Histopathology
Figure 5.31
Figure 5.32
Figure 5.33
Figure 5.34
Figure 5.35
Figure 5.36
Chapter 6: Eyelid Melanocytic Tumors
Eyelid Melanocytic Nevus
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Melanocytic Nevus: Pigmented Types
Figure 6.1
Figure 6.2
Figure 6.3
Figure 6.4
Figure 6.5
Figure 6.6
Eyelid Melanocytic Nevus: Age and Race Variations
Figure 6.7
Figure 6.8
Figure 6.9
Figure 6.10
Figure 6.11
Figure 6.12
Eyelid Melanocytic Nevus: Nonpigmented Types
Figure 6.13
Figure 6.14
Figure 6.15
Figure 6.16
Figure 6.17
Figure 6.18
Eyelid Melanocytic Nevus: Clinical Variations of Nonpigmented Type
Figure 6.19
Figure 6.20
Figure 6.21
Figure 6.22
Figure 6.23
Figure 6.24
Eyelid Melanocytic Nevus: Excision Technique and Pathology of Small Lesions
Figure 6.25
Figure 6.26
Figure 6.27
Figure 6.28
Figure 6.29
Figure 6.30
Eyelid Melanocytic Nevus: Congenital Divided (“Kissing”) Nevus
Figure 6.31
Figure 6.32
Figure 6.33
Figure 6.34
Figure 6.35
Figure 6.36
Eyelid Melanocytic Nevus: Large Congenital Periocular Type
Figure 6.37
Figure 6.38
Figure 6.39
Figure 6.40
Figure 6.41
Figure 6.42
Oculodermal Melanocytosis (Nevus of OTA)
General Considerations
Clinical Features
Pathology
Management
Selected References
Ocular Melanocytosis: Clinical Features
Figure 6.43
Figure 6.44
Figure 6.45
Figure 6.46
Figure 6.47
Figure 6.48
Congenital Oculodermal Melanocytosis: Spectrum of Pigmentation
Figure 6.49
Figure 6.50
Figure 6.51
Figure 6.52
Figure 6.53
Figure 6.54
Eyelid Lentigo Maligna (Melanotic Freckle of Hutchinson)
General Considerations
Clinical Features
Differential Diagnosis
Pathology
Management
Selected References
Eyelid Lentigo Maligna (Melanotic Freckle of Hutchinson)
Figure 6.55
Figure 6.56
Figure 6.57
Figure 6.58
Figure 6.59
Figure 6.60
Eyelid Lentigo Maligna: Surgical Excision
Figure 6.61
Figure 6.62
Figure 6.63
Figure 6.64
Figure 6.65
Figure 6.66
Eyelid Lentigo Maligna: Melanoma
Figure 6.67
Figure 6.68
Figure 6.69
Figure 6.70
Figure 6.71
Figure 6.72
Eyelid Blue Nevus
General Considerations
Clinical Features
Differential Diagnosis
Pathology
Management
Selected References
Eyelid Cellular Blue Nevus: Giving Rise to Orbital Melanoma
Figure 6.73
Figure 6.74
Figure 6.75
Figure 6.76
Figure 6.77
Figure 6.78
Eyelid Cellular Blue Nevus: Association with Orbital and Brain Melanoma
Figure 6.79
Figure 6.80
Figure 6.81
Figure 6.82
Figure 6.83
Figure 6.84
Figure 6.85
Figure 6.86
Figure 6.87
Figure 6.88
Figure 6.89
Figure 6.90
Eyelid Primary Malignant Melanoma
General Considerations
Clinical Features
Differential Diagnosis
Pathology and Pathogenesis
Management
Prognosis
Selected References
Primary Malignant Melanoma of Eyelid
Figure 6.91
Figure 6.92
Figure 6.93
Figure 6.94
Figure 6.95
Figure 6.96
Primary Eyelid Melanoma: Pigmented and Nonpigmented Varieties
Figure 6.97
Figure 6.98
Figure 6.99
Figure 6.100
Figure 6.101
Figure 6.102
Primary Eyelid Melanoma: Surgical Excision
Figure 6.103
Figure 6.104
Figure 6.105
Figure 6.106
Figure 6.107
Figure 6.108
Chapter 7: Neural Tumors of the Eyelid
Eyelid Neurofibroma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Neurofibroma: Localized and Plexiform Types
Figure 7.1
Figure 7.2
Figure 7.3
Figure 7.4
Figure 7.5
Figure 7.6
Eyelid Neurofibroma: Plexiform Type
Figure 7.7
Figure 7.8
Figure 7.9
Figure 7.10
Figure 7.11
Figure 7.12
Eyelid Schwannoma (Neurilemoma) and Neurothekeoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Schwannoma and Neurothekeoma
Figure 7.13
Figure 7.14
Figure 7.15
Figure 7.16
Figure 7.17
Figure 7.18
Eyelid Merkel Cell Carcinoma (Cutaneous Neuroendocrine Carcinoma)
General Considerations
Clinical Features
Classification
Differential Diagnosis
Pathology
Management
Selected References
Eyelid Merkel Cell Carcinoma (Cutaneous Neuroendocrine Carcinoma)
Figure 7.19
Figure 7.20
Figure 7.21
Figure 7.22
Figure 7.23
Figure 7.24
Eyelid Merkel Cell Carcinoma: Management and Clinicopathologic Correlation
Figure 7.25
Figure 7.26
Figure 7.27
Figure 7.28
Figure 7.29
Figure 7.30
Eyelid Merkel Cell Carcinoma: Clinical Appearance and Surgical Technique
Figure 7.31
Figure 7.32
Figure 7.33
Figure 7.34
Figure 7.35
Figure 7.36
Eyelid Merkel Cell Carcinoma: Pathology
Figure 7.37
Figure 7.38
Figure 7.39
Figure 7.40
Figure 7.41
Figure 7.42
Chapter 8: Vascular Tumors of the Eyelids
Eyelid Congenital Capillary Hemangioma (Strawberry Hemangioma)
General Considerations
Clinical Features
Complications
Differential Diagnosis
Pathology
Pathogenesis
Management
Selected References
Eyelid Congenital Capillary Hemangioma: Superficial Type
Figure 8.1
Figure 8.2
Figure 8.3
Figure 8.4
Figure 8.5
Figure 8.6
Eyelid Congenital Capillary Hemangioma: Deep Type
Figure 8.7
Figure 8.8
Figure 8.9
Figure 8.10
Figure 8.11
Figure 8.12
Eyelid Congenital Capillary Hemangioma: Regression of Superficial Type
Figure 8.13
Figure 8.14
Figure 8.15
Figure 8.16
Figure 8.17
Figure 8.18
Eyelid Congenital Capillary Hemangioma: Regression of Deep Type
Figure 8.19
Figure 8.20
Figure 8.21
Figure 8.22
Figure 8.23
Figure 8.24
Eyelid Congenital Capillary Hemangioma: Surgical Removal
Figure 8.25
Figure 8.26
Figure 8.27
Figure 8.28
Figure 8.29
Figure 8.30
Eyelid Acquired Hemangioma (Cherry Hemangioma)
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Acquired Capillary Hemangioma
Figure 8.31
Figure 8.32
Figure 8.33
Figure 8.34
Figure 8.35
Figure 8.36
Eyelid Nevus Flammeus (Port Wine Hemangioma)
General Considerations
Clinical Features
Pathology
Cytogenetics
Management
Selected References
Eyelid Nevus Flammeus (Port Wine Hemangioma)
Figure 8.37
Figure 8.38
Figure 8.39
Figure 8.40
Figure 8.41
Figure 8.42
Eyelid Nevus Flammeus: Clinical Variations and Follow-Up
Figure 8.43
Figure 8.44
Figure 8.45
Figure 8.46
Figure 8.47
Figure 8.48
Eyelid Nevus Flammeus: Association with Sturge–Weber Syndrome
Figure 8.49
Figure 8.50
Figure 8.51
Figure 8.52
Figure 8.53
Figure 8.54
Eyelid Varix
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Varix
Figure 8.55
Figure 8.56
Figure 8.57
Figure 8.58
Figure 8.59
Figure 8.60
Eyelid Lymphangioma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Lymphangioma
Figure 8.61
Figure 8.62
Figure 8.63
Figure 8.64
Figure 8.65
Figure 8.66
Eyelid Glomus Tumor
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Glomus Tumor
Figure 8.67
Figure 8.68
Figure 8.69
Figure 8.70
Figure 8.71
Figure 8.72
Eyelid Kaposi’s Sarcoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Kaposi’s Sarcoma in a Nonimmunosuppressed Patient
Figure 8.73
Figure 8.74
Figure 8.75
Figure 8.76
Figure 8.77
Figure 8.78
Eyelid Kaposi’s Sarcoma in Immunosuppressed Patients
Figure 8.79
Figure 8.80
Figure 8.81
Figure 8.82
Figure 8.83
Figure 8.84
Eyelid Kaposi’s Sarcoma: Treatment with Radiotherapy
Figure 8.85
Figure 8.86
Figure 8.87
Figure 8.88
Figure 8.89
Figure 8.90
Eyelid Angiosarcoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Angiosarcoma: Clinical Variations
Figure 8.91
Figure 8.92
Figure 8.93
Figure 8.94
Figure 8.95
Figure 8.96
Chapter 9: Eyelid Lymphoid, Plasmacytic, and Metastatic Tumors
Eyelid Lymphoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Involvement: B-Cell Lymphoma
Figure 9.1
Figure 9.2
Figure 9.3
Figure 9.4
Figure 9.5
Figure 9.6
Figure 9.7
Figure 9.8
Figure 9.9
Figure 9.10
Figure 9.11
Figure 9.12
Eyelid Involvement by Lymphoma: Advanced Cases
Figure 9.13
Figure 9.14
Figure 9.15
Figure 9.16
Figure 9.17
Figure 9.18
Eyelid Involvement: T-Cell Lymphoma
Figure 9.19
Figure 9.20
Figure 9.21
Figure 9.22
Figure 9.23
Figure 9.24
Eyelid Plasmacytoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Figure 9.25
Figure 9.26
Figure 9.27
Figure 9.28
Figure 9.29
Figure 9.30
Metastatic Neoplasms to the Eyelids
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Metastatic Tumors
Figure 9.31
Figure 9.32
Figure 9.33
Figure 9.34
Figure 9.35
Figure 9.36
Figure 9.37
Figure 9.38
Figure 9.39
Figure 9.40
Figure 9.41
Figure 9.42
Eyelid Metastatic Tumors from Choroidal Melanoma
Figure 9.43
Figure 9.44
Figure 9.45
Figure 9.46
Figure 9.47
Figure 9.48
Chapter 10: Eyelid Histiocytic, Myxoid, and Fibrous Lesions
Eyelid Histiocytic, Myxoid, and Fibrous Lesions
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Xanthelasma
Figure 10.1
Figure 10.2
Figure 10.3
Figure 10.4
Figure 10.5
Figure 10.6
Eyelid Xanthelasma: Association with Systemic Conditions
Figure 10.7
Figure 10.8
Figure 10.9
Figure 10.10
Figure 10.11
Figure 10.12
Eyelid Xanthogranuloma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Juvenile Xanthogranuloma
Figure 10.13
Figure 10.14
Figure 10.15
Figure 10.16
Figure 10.17
Figure 10.18
Eyelid Necrobiotic Xanthogranuloma with Paraproteinemia
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Necrobiotic Xanthogranuloma with Paraproteinemia
Figure 10.19
Figure 10.20
Figure 10.21
Figure 10.22
Figure 10.23
Figure 10.24
Eyelid Angiofibroma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid and Facial Angiofibroma with Tuberous Sclerosis Complex
Figure 10.25
Figure 10.26
Figure 10.27
Figure 10.28
Figure 10.29
Figure 10.30
Eyelid Nodular Fasciitis
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Nodular Fasciitis
Figure 10.31
Figure 10.32
Figure 10.33
Figure 10.34
Figure 10.35
Figure 10.36
Eyelid Nodular Fasciitis: Clinicopathologic Correlation
Figure 10.37
Figure 10.38
Figure 10.39
Figure 10.40
Figure 10.41
Figure 10.42
Eyelid Miscellaneous Fibrous and Myxomatous Tumors
Juvenile Fibromatosis
Fibrous Histiocytoma
Fibrosarcoma
Myxoma
Multicentric Reticulohistiocytosis
Selected References
Eyelid Juvenile Fibromatosis, Fibrous Histiocytoma, and Fibrosarcoma
Figure 10.43
Figure 10.44
Figure 10.45
Figure 10.46
Figure 10.47
Figure 10.48
Eyelid Myxoma and Multicentric Reticulohistiocytosis
Figure 10.49
Figure 10.50
Figure 10.51
Figure 10.52
Figure 10.53
Figure 10.54
Chapter 11: Eyelid Cystic Lesions Simulating Neoplasms
Eyelid Eccrine Hidrocystoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Eccrine Hidrocystoma
Figure 11.1
Figure 11.2
Figure 11.3
Figure 11.4
Figure 11.5
Figure 11.6
Eyelid Apocrine Hidrocystoma
General Considerations
Clinical Features
Schöpf–Schulz–Passarge Syndrome
Pathology
Management
Selected References
Eyelid Apocrine Hidrocystoma
Figure 11.7
Figure 11.8
Figure 11.9
Figure 11.10
Figure 11.11
Figure 11.12
Eyelid Sebaceous Cyst (Pilar Cyst)
Sebaceous Cyst
Clinical Features
Pathology
Management
Selected References
Eyelid Sebaceous Cyst
Figure 11.13
Figure 11.14
Figure 11.15
Figure 11.16
Figure 11.17
Figure 11.18
Eyelid Epidermal Inclusion Cyst (Epidermoid Cyst)
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Epidermal Inclusion Cyst
Figure 11.19
Figure 11.20
Figure 11.21
Figure 11.22
Figure 11.23
Figure 11.24
Eyelid Dermoid Cyst
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid/Orbital Dermoid Cyst: Clinicopathologic Correlation
Figure 11.25
Figure 11.26
Figure 11.27
Figure 11.28
Figure 11.29
Figure 11.30
Chapter 12: Eyelid Inflammatory Lesions Simulating Neoplasms
Eyelid Molluscum Contagiosum Infection
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Molluscum Contagiosum Infection
Figure 12.1
Figure 12.2
Figure 12.3
Figure 12.4
Figure 12.5
Figure 12.6
Eyelid Chalazion
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Chalazion
Figure 12.7
Figure 12.8
Figure 12.9
Figure 12.10
Figure 12.11
Figure 12.12
Eyelid Chalazion: Clinical Variations
Figure 12.13
Figure 12.14
Figure 12.15
Figure 12.16
Figure 12.17
Figure 12.18
Miscellaneous Granulomatous Diseases
Eyelid Sarcoidosis
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Pseudorheumatoid Nodule (Granuloma Annulare)
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Granulomatosis with Polyangiitis (Wegener’s Granulomatosis)
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Granulomas: Sarcoidosis, Pseudorheumatoid Nodule, and Granulomatosis with Polyangiitis (Wegener Granulomatosis)
Figure 12.19
Figure 12.20
Figure 12.21
Figure 12.22
Figure 12.23
Figure 12.24
Eyelid Mycotic Infections
Eyelid Blastomycosis
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Coccidioidomycosis
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Mucormycosis
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Mycotic Infections: Coccidioidomycosis and Mucormycosis
Figure 12.25
Figure 12.26
Figure 12.27
Figure 12.28
Figure 12.29
Figure 12.30
Eyelid Bacterial Infections
Eyelid Abscess
General Considerations
Clinical Features
Pathology
Management
Necrotizing Fasciitis Involving Eyelid
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Bacterial Infections: Abscess and Necrotizing Fasciitis
Figure 12.31
Figure 12.32
Figure 12.33
Figure 12.34
Figure 12.35
Figure 12.36
Chapter 13: Eyelid Miscellaneous Conditions Simulating Neoplasms
Eyelid Amyloidosis
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Amyloidosis
Figure 13.1
Figure 13.2
Figure 13.3
Figure 13.4
Figure 13.5
Figure 13.6
Eyelid Lipoid Proteinosis (Urbach–Wiethe Disease)
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Lipoid Proteinosis (Urbach–Wiethe Disease)
Figure 13.7
Figure 13.8
Figure 13.9
Figure 13.10
Figure 13.11
Figure 13.12
Miscellaneous Other Pseudoneoplastic Eyelid Lesions
Eyelid Granular Cell Tumor
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Malakoplakia
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Subepidermal Calcified Nodule
General Considerations
Clinical Features
Pathology
Management
Selected References
Miscellaneous Eyelid Lesions: Granular Cell Tumor, Malakoplakia, and Subepidermal Calcified Nodule
Figure 13.13
Figure 13.14
Figure 13.15
Figure 13.16
Figure 13.17
Figure 13.18
Eyelid Phakomatous Choristoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Eyelid Phakomatous Choristoma
Figure 13.19
Figure 13.20
Figure 13.21
Figure 13.22
Figure 13.23
Figure 13.24
Chapter 14: Tumors of the Lacrimal Drainage System
Lacrimal Drainage System Tumors
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Lacrimal Sac Squamous Papilloma and Carcinoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Lacrimal Sac Squamous Cell Papilloma and Carcinoma
Figure 14.1
Figure 14.2
Figure 14.3
Figure 14.4
Figure 14.5
Figure 14.6
Lacrimal Sac Melanoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Lacrimal Sac Melanoma
Figure 14.7
Figure 14.8
Figure 14.9
Figure 14.10
Figure 14.11
Figure 14.12
Lacrimal Sac: Miscellaneous Tumors and Pseudotumors
Selected References
Miscellaneous Lacrimal Sac Tumors: Leiomyoma, Fibrous Histiocytoma, and Lymphoma
Figure 14.13
Figure 14.14
Figure 14.15
Figure 14.16
Figure 14.17
Figure 14.18
Lacrimal Sac Inflammations and Infections
Figure 14.19
Figure 14.20
Figure 14.21
Figure 14.22
Figure 14.23
Figure 14.24
Chapter 15: Surgical Management of Eyelid Tumors
Surgical Management of Eyelid Tumors
Selected References
Punch Biopsy, Excisional Shave Biopsy, and Elliptical Excision with Skin Graft
Figure 15.1
Figure 15.2
Figure 15.3
Figure 15.4
Figure 15.5
Figure 15.6
Elliptical Excision of Eyelid Tumor
Figure 15.7
Figure 15.8
Figure 15.9
Figure 15.10
Figure 15.11
Figure 15.12
Pentagonal Full-Thickness Excision of Eyelid Tumor with Semicircular Flap Reconstruction
Figure 15.13
Figure 15.14
Figure 15.15
Figure 15.16
Figure 15.17
Figure 15.18
Pentagonal Full-Thickness Excision of Eyelid Tumor with Primary Closure
Figure 15.19
Figure 15.20
Figure 15.21
Figure 15.22
Figure 15.23
Figure 15.24
Part 2: Tumors of the Conjunctiva
Chapter 16: Conjunctival and Epibulbar Choristomas
Conjunctival Dermoid
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Dermoid
Figure 16.1
Figure 16.2
Figure 16.3
Figure 16.4
Figure 16.5
Figure 16.6
Conjunctival and Corneal Dermoids
Figure 16.7
Figure 16.8
Figure 16.9
Figure 16.10
Figure 16.11
Figure 16.12
Conjunctival and Corneal Dermoids: Atypical Variations
Figure 16.13
Figure 16.14
Figure 16.15
Figure 16.16
Figure 16.17
Figure 16.18
Conjunctival/Orbital Dermolipoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Dermolipoma
Figure 16.19
Figure 16.20
Figure 16.21
Figure 16.22
Figure 16.23
Figure 16.24
Conjunctival Dermoids and Dermolipomas: Bilobed and Pedunculated Variants
Figure 16.25
Figure 16.26
Figure 16.27
Figure 16.28
Figure 16.29
Figure 16.30
Epibulbar Osseous Choristoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Epibulbar Osseous Choristoma
Figure 16.31
Figure 16.32
Figure 16.33
Figure 16.34
Figure 16.35
Figure 16.36
Lacrimal Gland and Respiratory Choristomas of Conjunctiva
General Considerations
Clinical Features
Pathology
Management
Selected References
Lacrimal Gland and Respiratory Choristomas of Conjunctiva
Figure 16.37
Figure 16.38
Figure 16.39
Figure 16.40
Figure 16.41
Figure 16.42
Conjunctival Complex Choristoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Epibulbar Complex Choristoma: Association with Organoid Nevus Syndrome
Figure 16.43
Figure 16.44
Figure 16.45
Figure 16.46
Figure 16.47
Figure 16.48
Figure 16.49
Figure 16.50
Figure 16.51
Figure 16.52
Figure 16.53
Figure 16.54
Chapter 17: Conjunctival Benign Epithelial Tumors
Conjunctival Papilloma of Childhood
General Considerations
Clinical Features
Pathology and Pathogenesis
Management
Selected References
Childhood Conjunctival Papilloma
Figure 17.1
Figure 17.2
Figure 17.3
Figure 17.4
Figure 17.5
Figure 17.6
Conjunctival Papilloma of Childhood: Management with Oral Cimetidine
Figure 17.7
Figure 17.8
Figure 17.9
Figure 17.10
Figure 17.11
Figure 17.12
Conjunctival Papilloma of Adulthood
General Considerations
Clinical Features
Pathology
Management
Selected References
Adult Conjunctival Papilloma
Figure 17.13
Figure 17.14
Figure 17.15
Figure 17.16
Figure 17.17
Figure 17.18
Adult Conjunctival Papilloma: Atypical Variations
Figure 17.19
Figure 17.20
Figure 17.21
Figure 17.22
Figure 17.23
Figure 17.24
Conjunctival Pseudoepitheliomatous Hyperplasia and Keratoacanthoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Pseudoepitheliomatous Hyperplasia and Keratoacanthoma
Figure 17.25
Figure 17.26
Figure 17.27
Figure 17.28
Figure 17.29
Figure 17.30
Conjunctival Hereditary Benign Intraepithelial Dyskeratosis
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Hereditary Benign Intraepithelial Dyskeratosis
Figure 17.31
Figure 17.32
Figure 17.33
Figure 17.34
Figure 17.35
Figure 17.36
Conjunctival Dacryoadenoma
General Considerations
Clinical Features
Pathology
Management
Selected Reference
Conjunctival Dacryoadenoma
Figure 17.37
Figure 17.38
Figure 17.39
Figure 17.40
Figure 17.41
Figure 17.42
Chapter 18: Premalignant and Malignant Lesions of the Conjunctival Epithelium
Conjunctival Keratotic Plaque and Actinic Keratosis
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Keratotic Plaque and Actinic Keratosis
Figure 18.1
Figure 18.2
Figure 18.3
Figure 18.4
Figure 18.5
Figure 18.6
Conjunctival Intraepithelial Neoplasia
General Considerations
Clinical Features
Diagnosis
Pathology
Management
Selected References
Conjunctival Intraepithelial Neoplasia: Fleshy and Papillomatous Configurations
Figure 18.7
Figure 18.8
Figure 18.9
Figure 18.10
Figure 18.11
Figure 18.12
Conjunctival Intraepithelial Neoplasia (Cin): Leukoplakia
Figure 18.13
Figure 18.14
Figure 18.15
Figure 18.16
Figure 18.17
Figure 18.18
Conjunctival Intraepithelial Neoplasia: Various Clinical Locations at Limbus
Figure 18.19
Figure 18.20
Figure 18.21
Figure 18.22
Figure 18.23
Figure 18.24
Conjunctival Intraepithelial Neoplasia: Superficial Corneal Invasion
Figure 18.25
Figure 18.26
Figure 18.27
Figure 18.28
Figure 18.29
Figure 18.30
Conjunctival Invasive Squamous Cell Carcinoma
General Considerations
Clinical Features
Diagnosis
Pathology
Classification
Management
Prognosis
Selected References
Table 18.1: American Joint Committee on Cancer (AJCC) classification of ocular surface squamous neoplasia
Conjunctival Squamous Cell Carcinoma: Sunlight Exposure
Figure 18.31
Figure 18.32
Figure 18.33
Figure 18.34
Figure 18.35
Figure 18.36
Conjunctival Squamous Cell Carcinoma: Early Invasive Type
Figure 18.37
Figure 18.38
Figure 18.39
Figure 18.40
Figure 18.41
Figure 18.42
Conjunctival Squamous Cell Carcinoma: Advanced Invasive Type
Figure 18.43
Figure 18.44
Figure 18.45
Figure 18.46
Figure 18.47
Figure 18.48
Conjunctival Squamous Cell Carcinoma: Involvement Of Tarsal Conjunctiva
Figure 18.49
Figure 18.50
Figure 18.51
Figure 18.52
Figure 18.53
Figure 18.54
Conjunctival Squamous Cell Carcinoma: Extensive Papillomatous Corneal Involvement
Figure 18.55
Figure 18.56
Figure 18.57
Figure 18.58
Figure 18.59
Figure 18.60
Conjunctival Squamous Cell Carcinoma: Atypical Variations
Figure 18.61
Figure 18.62
Figure 18.63
Figure 18.64
Figure 18.65
Figure 18.66
Conjunctival Spindle Cell Carcinoma: En Bloc Eye Wall Resection
Figure 18.67
Figure 18.68
Figure 18.69
Figure 18.70
Figure 18.71
Figure 18.72
Conjunctival Squamous Cell Carcinoma: Orbital Invasion
Figure 18.73
Figure 18.74
Figure 18.75
Figure 18.76
Figure 18.77
Figure 18.78
Conjunctival Squamous Cell Carcinoma: Intraocular Invasion
Figure 18.79
Figure 18.80
Figure 18.81
Figure 18.82
Figure 18.83
Figure 18.84
Conjunctival Mucoepidermoid Squamous Cell Carcinoma: Intraocular Invasion
Figure 18.85
Figure 18.86
Figure 18.87
Figure 18.88
Figure 18.89
Figure 18.90
Chapter 19: Conjunctival Melanocytic Lesions
Conjunctival Melanocytic Nevus
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Melanocytic Nevus: Pigmented Type
Figure 19.1
Figure 19.2
Figure 19.3
Figure 19.4
Figure 19.5
Figure 19.6
Conjunctival Melanocytic Nevus: Nonpigmented Type
Figure 19.7
Figure 19.8
Figure 19.9
Figure 19.10
Figure 19.11
Figure 19.12
Conjunctival Melanocytic Nevus: Partially Pigmented Type
Figure 19.13
Figure 19.14
Figure 19.15
Figure 19.16
Figure 19.17
Figure 19.18
Conjunctival Melanocytic Nevus: Clinical Variations
Figure 19.19
Figure 19.20
Figure 19.21
Figure 19.22
Figure 19.23
Figure 19.24
Conjunctival Melanocytic Nevus: Extralimbal Location
Figure 19.25
Figure 19.26
Figure 19.27
Figure 19.28
Figure 19.29
Figure 19.30
Conjunctival Melanocytic Nevus: Atypical Cases with Prominent Cysts and Large Size (Giant Nevus)
Figure 19.31
Figure 19.32
Figure 19.33
Figure 19.34
Figure 19.35
Figure 19.36
Conjunctival Melanocytic Nevus: Blue Nevus Variant
Figure 19.37
Figure 19.38
Figure 19.39
Figure 19.40
Figure 19.41
Figure 19.42
Conjunctival Melanocytic Nevus: Giant Type
Figure 19.43
Figure 19.44
Figure 19.45
Figure 19.46
Figure 19.47
Figure 19.48
Conjunctival Melanocytic Nevus in Non-Caucasians
Figure 19.49
Figure 19.50
Figure 19.51
Figure 19.52
Figure 19.53
Figure 19.54
Ocular Melanocytosis: Scleral and Episcleral Pigment
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Scleral Involvement with Congenital Ocular Melanocytosis
Figure 19.55
Figure 19.56
Figure 19.57
Figure 19.58
Figure 19.59
Figure 19.60
Complexion-Related Conjunctival Pigmentation (Complexion-Associated Melanosis, Racial Melanosis)
General Considerations
Clinical Features
Pathology
Management
Selected References
Complexion-Related Conjunctival Pigmentation (“Racial Melanosis”)
Figure 19.61
Figure 19.62
Figure 19.63
Figure 19.64
Figure 19.65
Figure 19.66
Conjunctival Primary Acquired Melanosis
General Considerations
Clinical Features
Pathology
Management
Selected References
Table 19.1: Differential diagnosis of pigmented conjunctival and epibulbar lesions
Conjunctival Primary Acquired Melanosis: Mild Involvement
Figure 19.67
Figure 19.68
Figure 19.69
Figure 19.70
Figure 19.71
Figure 19.72
Conjunctival Primary Acquired Melanosis: Severe Atypia
Figure 19.73
Figure 19.74
Figure 19.75
Figure 19.76
Figure 19.77
Figure 19.78
Conjunctival Primary Acquired Melanosis: Development of Early Melanoma
Figure 19.79
Figure 19.80
Figure 19.81
Figure 19.82
Figure 19.83
Figure 19.84
Conjunctival Primary Acquired Melanosis: Development of Obvious Melanoma
Figure 19.85
Figure 19.86
Figure 19.87
Figure 19.88
Figure 19.89
Figure 19.90
Conjunctival Malignant Melanoma
General Considerations
Clinical Features
Differential Diagnosis
Pathology
Management
Prognosis
Selected References
Table 19.2: American Joint Committee on Cancer (AJCC) classification of conjunctival melanoma
Conjunctival Melanoma: Evolution from Primary Acquired Melanosis
Figure 19.91
Figure 19.92
Figure 19.93
Figure 19.94
Figure 19.95
Figure 19.96
Figure 19.97
Figure 19.98
Figure 19.99
Figure 19.100
Figure 19.101
Figure 19.102
Conjunctival Melanoma in Non-Caucasians
Figure 19.103
Figure 19.104
Figure 19.105
Figure 19.106
Figure 19.107
Figure 19.108
Conjunctival Melanoma: Tumors Possibly Arising De Novo
Figure 19.109
Figure 19.110
Figure 19.111
Figure 19.112
Figure 19.113
Figure 19.114
Conjunctival Melanoma: Presumably Arising from Nevus and De Novo
Figure 19.115
Figure 19.116
Figure 19.117
Figure 19.118
Figure 19.119
Figure 19.120
Conjunctival Melanoma: Amelanotic Variations
Figure 19.121
Figure 19.122
Figure 19.123
Figure 19.124
Figure 19.125
Figure 19.126
Conjunctival Melanoma: Alcohol Epitheliectomy, Surgical Resection, and Cryotherapy. Results of Treatment
Figure 19.127
Figure 19.128
Figure 19.129
Figure 19.130
Figure 19.131
Figure 19.132
Conjunctival Melanoma: Diffuse Tumors before and after Treatment
Figure 19.133
Figure 19.134
Figure 19.135
Figure 19.136
Figure 19.137
Figure 19.138
Conjunctival Melanoma: Clinicopathologic Correlation of Tumor with Scleral Invasion
Figure 19.139
Figure 19.140
Figure 19.141
Figure 19.142
Figure 19.143
Figure 19.144
Conjunctival Melanoma: Localization for Sentinel Lymph Node Biopsy
Figure 19.145
Figure 19.146
Figure 19.147
Figure 19.148
Figure 19.149
Figure 19.150
Conjunctival Melanoma: Plaque Radiotherapy for Advanced, Recurrent Tumor
Figure 19.151
Figure 19.152
Figure 19.153
Figure 19.154
Figure 19.155
Figure 19.156
Conjunctival Melanoma: Orbital Exenteration
Figure 19.157
Figure 19.158
Figure 19.159
Figure 19.160
Figure 19.161
Figure 19.162
Conjunctival Melanoma: Metastasis to Preauricular Lymph Nodes and Brain
Figure 19.163
Figure 19.164
Figure 19.165
Figure 19.166
Figure 19.167
Figure 19.168
Chapter 20: Vascular Tumors and Related Lesions of the Conjunctiva
Conjunctival Pyogenic Granuloma
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Pyogenic Granuloma: Primary (Idiopathic) Type
Figure 20.1
Figure 20.2
Figure 20.3
Figure 20.4
Figure 20.5
Figure 20.6
Secondary Conjunctival Pyogenic Granuloma: Treatment with Plaque Radiotherapy
Figure 20.7
Figure 20.8
Figure 20.9
Figure 20.10
Figure 20.11
Figure 20.12
Conjunctival Lymphangiectasia and Lymphangioma
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Lymphangiectasia and Lymphangioma
Figure 20.13
Figure 20.14
Figure 20.15
Figure 20.16
Figure 20.17
Figure 20.18
Conjunctival Lymphangioma
Figure 20.19
Figure 20.20
Figure 20.21
Figure 20.22
Figure 20.23
Figure 20.24
Miscellaneous Vascular Lesions of the Conjunctiva: Varix, Cavernous Hemangioma, Macrovessels, Sentinel Vessels, and Acquired Sessile Hemangioma
Conjunctival Varix
General Considerations
Clinical Features
Pathology
Management
Cavernous Hemangioma
General Considerations
Clinical Features
Pathology
Management
Conjunctival Macrovessels and Episcleral Sentinel Vessels
Selected References
Conjunctival Varix, Cavernous Hemangioma, Macrovessels, and Sentinel Vessels
Figure 20.25
Figure 20.26
Figure 20.27
Figure 20.28
Figure 20.29
Figure 20.30
Conjunctival Acquired Sessile Hemangioma and Capillary Hemangioma
Acquired Sessile Hemangioma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Conjunctival Capillary Hemangioma
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Congenital Capillary Hemangioma, Acquired Sessile Hemangioma, and Varix
Figure 20.31
Figure 20.32
Figure 20.33
Figure 20.34
Figure 20.35
Figure 20.36
Conjunctival Hemangiopericytoma And Glomangioma (Glomus Tumor)
Conjunctival Hemangiopericytoma
General Considerations
Clinical Features
Pathology
Management
Conjunctival Glomangioma (Glomus Tumor)
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Hemangiopericytoma and Glomangioma
Figure 20.37
Figure 20.38
Figure 20.39
Figure 20.40
Figure 20.41
Figure 20.42
Conjunctival Kaposi Sarcoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Kaposi Sarcoma in Patients with AIDS and Immunocompetent Patients
Figure 20.43
Figure 20.44
Figure 20.45
Figure 20.46
Figure 20.47
Figure 20.48
Chapter 21: Conjunctival Neural, Xanthomatous, Fibrous, Myxomatous, and Lipomatous Tumors
Conjunctival Neuroma and Neurofibroma
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Neurofibroma
Figure 21.1
Figure 21.2
Figure 21.3
Figure 21.4
Figure 21.5
Figure 21.6
Conjunctival Schwannoma and Granular Cell Tumor: Conjunctival Schwannoma
Conjunctival Schwannoma
General Considerations
Clinical Features
Pathology
Management
Conjunctival Granular Cell Tumor
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Schwannoma and Granular Cell Tumor
Figure 21.7
Figure 21.8
Figure 21.9
Figure 21.10
Figure 21.11
Figure 21.12
Conjunctival Fibrous Histiocytoma: General Considerations
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Fibrous Histiocytoma
Figure 21.13
Figure 21.14
Figure 21.15
Figure 21.16
Figure 21.17
Figure 21.18
Conjunctival Miscellaneous Lesions: Fibroma, Nodular Fasciitis, and Juvenile Xanthogranuloma: Conjunctival Fibroma
Conjunctival Fibroma
General Considerations
Clinical Features
Pathology
Management
Conjunctival Nodular Fasciitis
General Considerations
Clinical Features
Pathology
Management
Conjunctival Juvenile Xanthogranuloma
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Nodular Fasciitis and Juvenile Xanthogranuloma
Figure 21.19
Figure 21.20
Figure 21.21
Figure 21.22
Figure 21.23
Figure 21.24
Conjunctival Miscellaneous Lesions: Myxoma, Lipoma, and Reticulohistiocytoma: Conjunctival Myxoma
Conjunctival Myxoma
General Considerations
Clinical Features
Carney Complex
Pathology
Management
Conjunctival Lipoma
General Considerations
Clinical Features
Pathology
Management
Conjunctival Reticulohistiocytoma
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Myxoma, Lipoma, and Reticulohistiocytoma
Figure 21.25
Figure 21.26
Figure 21.27
Figure 21.28
Figure 21.29
Figure 21.30
Chapter 22: Conjunctival Lymphoid, Leukemic, and Metastatic Tumors
Conjunctival Lymphoid and Plasmacytic Tumors
General Considerations
Clinical Features
Pathology
Management
Selected References
Table 22.1: American Joint Committee on Cancer (AJCC) classification of ocular adnexal lymphoma
Conjunctival Benign Reactive Lymphoid Hyperplasia
Figure 22.1
Figure 22.2
Figure 22.3
Figure 22.4
Figure 22.5
Figure 22.6
Conjunctival Non-Hodgkin’s Lymphoma
Figure 22.7
Figure 22.8
Figure 22.9
Figure 22.10
Figure 22.11
Figure 22.12
Conjunctival Lymphoma: Atypical Forms and Response to Radiotherapy
Figure 22.13
Figure 22.14
Figure 22.15
Figure 22.16
Figure 22.17
Figure 22.18
Conjunctival Posttransplant Lymphoproliferative Disorder
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Posttransplant Lymphoproliferative Disorder
Figure 22.19
Figure 22.20
Figure 22.21
Figure 22.22
Figure 22.23
Figure 22.24
Conjunctival Leukemia
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Leukemic Infiltrate
Figure 22.25
Figure 22.26
Figure 22.27
Figure 22.28
Figure 22.29
Figure 22.30
Conjunctival Metastatic Tumors
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Metastasis
Figure 22.31
Figure 22.32
Figure 22.33
Figure 22.34
Figure 22.35
Figure 22.36
Conjunctival Metastasis from Cutaneous Melanoma
Figure 22.37
Figure 22.38
Figure 22.39
Figure 22.40
Figure 22.41
Figure 22.42
Chapter 23: Caruncular Tumors
Caruncular Tumors
General Considerations
Clinical Features
Pathology
Management
Selected References
Table 23.1: Types of tumors in the caruncle in a series of 93 cases
Caruncular Papilloma
Figure 23.1
Figure 23.2
Figure 23.3
Figure 23.4
Figure 23.5
Figure 23.6
Caruncular Nevus
Figure 23.7
Figure 23.8
Figure 23.9
Figure 23.10
Figure 23.11
Figure 23.12
Caruncular Melanoma
Figure 23.13
Figure 23.14
Figure 23.15
Figure 23.16
Figure 23.17
Figure 23.18
Caruncular Oncocytoma
Figure 23.19
Figure 23.20
Figure 23.21
Figure 23.22
Figure 23.23
Figure 23.24
Caruncular Sebaceous Tumors
Figure 23.25
Figure 23.26
Figure 23.27
Figure 23.28
Figure 23.29
Figure 23.30
Caruncular Cysts
Figure 23.31
Figure 23.32
Figure 23.33
Figure 23.34
Figure 23.35
Figure 23.36
Miscellaneous Caruncular Tumors
Figure 23.37
Figure 23.38
Figure 23.39
Figure 23.40
Figure 23.41
Figure 23.42
Chapter 24: Miscellaneous Lesions That Simulate Conjunctival Neoplasms
Conjunctival Epithelial Inclusion Cyst
General Considerations
Clinical Features
Pathology
Management
Selected References
Figure 24.1
Figure 24.2
Figure 24.3
Figure 24.4
Figure 24.5
Figure 24.6
Conjunctival Organizing Hematoma (“Hematic Cyst”; “Hematocele”)
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Organizing Hematoma Secondary to Silicone Sponge for Retinal Detachment Repair
Figure 24.7
Figure 24.8
Figure 24.9
Figure 24.10
Figure 24.11
Figure 24.12
Conjunctival Foreign Body
General Considerations
Clinical Features
Pathology
Management
Selected References
Figure 24.13
Figure 24.14
Figure 24.15
Figure 24.16
Figure 24.17
Figure 24.18
Figure 24.19
Figure 24.20
Figure 24.21
Figure 24.22
Figure 24.23
Figure 24.24
Episcleritis and Scleritis Simulating Neoplasms
General Considerations
Clinical Features
Pathology
Management
Selected References
Episcleritis and Scleritis
Figure 24.25
Figure 24.26
Figure 24.27
Figure 24.28
Figure 24.29
Figure 24.30
Conjunctival Churg–Strauss Allergic Granulomatosis Simulating Conjunctival Neoplasm
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Churg–Strauss Allergic Granulomatosis
Figure 24.31
Figure 24.32
Figure 24.33
Figure 24.34
Figure 24.35
Figure 24.36
Conjunctival Ligneous Conjunctivitis
General Considerations
Clinical Features
Pathology
Management
Selected References
Figure 24.37
Figure 24.38
Figure 24.39
Figure 24.40
Figure 24.41
Figure 24.42
Conjunctival Miscellaneous Infectious Lesions that Simulate Neoplasms
Selected References
Figure 24.43
Figure 24.44
Figure 24.45
Figure 24.46
Figure 24.47
Figure 24.48
Figure 24.49
Figure 24.50
Figure 24.51
Figure 24.52
Figure 24.53
Figure 24.54
Conjunctival Amyloidosis
General Considerations
Clinical Features
Pathology
Management
Selected References
Figure 24.55
Figure 24.56
Figure 24.57
Figure 24.58
Figure 24.59
Figure 24.60
Figure 24.61
Figure 24.62
Figure 24.63
Figure 24.64
Figure 24.65
Figure 24.66
Pinguecula
General Considerations
Clinical Features
Pathology
Management
Selected References
Conjunctival Pinguecula
Figure 24.67
Figure 24.68
Figure 24.69
Figure 24.70
Figure 24.71
Figure 24.72
Pterygium
General Considerations
Clinical Features
Pathology
Management
Selected References
Figure 24.73
Figure 24.74
Figure 24.75
Figure 24.76
Figure 24.77
Figure 24.78
Conjunctival and Scleral Miscellaneous Lesions that Simulate Pigmented Melanoma
Calcified Scleral Plaque
Staphyloma
Extraocular Extension of Ciliary Body Melanoma
Selected References
Scleral Staphyloma and Uveal Prolapse that Simulate Melanoma
Figure 24.79
Figure 24.80
Figure 24.81
Figure 24.82
Figure 24.83
Figure 24.84
Conjunctival Miscellaneous Lesions that Simulate Melanoma
Figure 24.85
Figure 24.86
Figure 24.87
Figure 24.88
Figure 24.89
Figure 24.90
Chapter 25: Surgical Management of Conjunctival Tumors
Surgical Management of Conjunctival Tumors
Selected References
Surgical Resection of Circumscribed Conjunctival Tumors Near Limbus
Figure 25.1
Figure 25.2
Figure 25.3
Figure 25.4
Figure 25.5
Figure 25.6
Surgical Management of Primary Acquired Melanosis and Melanoma of Conjunctiva
Figure 25.7
Figure 25.8
Figure 25.9
Figure 25.10
Figure 25.11
Figure 25.12
Results of Surgical Management of Conjunctival Tumors
Figure 25.13
Figure 25.14
Figure 25.15
Figure 25.16
Figure 25.17
Figure 25.18
Treatment of Conjunctival Malignancies with Topical Chemotherapy and Interferon
Figure 25.19
Figure 25.20
Figure 25.21
Figure 25.22
Figure 25.23
Figure 25.24
Supplemental Treatment of Conjunctival Neoplasms with Plaque Radiotherapy
Figure 25.25
Figure 25.26
Figure 25.27
Figure 25.28
Figure 25.29
Figure 25.30
Supplemental Treatment of Extensive Conjunctival Neoplasm with Plaque Brachytherapy
Figure 25.31
Figure 25.32
Figure 25.33
Figure 25.34
Figure 25.35
Figure 25.36
Part 3: Tumors of the Orbit
Chapter 26: Inflammatory Orbital Lesions That Simulate Neoplasms
Thyroid-Related Ophthalmopathy
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 26.1
Figure 26.2
Figure 26.3
Figure 26.4
Figure 26.5
Figure 26.6
Thyroid-Related Ophthalmopathy: Clinical and Radiologic Variations
Figure 26.7
Figure 26.8
Figure 26.9
Figure 26.10
Figure 26.11
Figure 26.12
Orbital Cellulitis
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Cellulitis and Abscess
Figure 26.13
Figure 26.14
Figure 26.15
Figure 26.16
Figure 26.17
Figure 26.18
Orbit: Idiopathic Nongranulomatous Orbital Inflammation (Inflammatory Pseudotumor, Idiopathic Orbital Inflammatory Syndrome)
General Considerations
Clinical Features
Differential Diagnosis
Diagnostic Approaches
Pathology
Management
Selected References
Idiopathic Nongranulomatous Orbital Inflammation in Adulthood
Figure 26.19
Figure 26.20
Figure 26.21
Figure 26.22
Figure 26.23
Figure 26.24
Idiopathic Nongranulomatous Orbital Inflammation Clinical and Radiologic Spectrum
Figure 26.25
Figure 26.26
Figure 26.27
Figure 26.28
Figure 26.29
Figure 26.30
Idiopathic Nongranulomatous Orbital Inflammation in Childhood
Figure 26.31
Figure 26.32
Figure 26.33
Figure 26.34
Figure 26.35
Figure 26.36
Nonspecific Acute Orbital Myositis
Figure 26.37
Figure 26.38
Figure 26.39
Figure 26.40
Figure 26.41
Figure 26.42
Immunoglobulin G4–Related Disease (IgG4-RD)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Tuberculosis
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 26.43
Figure 26.44
Figure 26.45
Figure 26.46
Figure 26.47
Figure 26.48
Orbital Mycotic Infections: Aspergillosis and Mucormycosis
Orbital Mucormycosis
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Aspergillosis—Allergic Fungal Sinusitis
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Mycotic Infections: Aspergillosis and Mucormycosis
Figure 26.49
Figure 26.50
Figure 26.51
Figure 26.52
Figure 26.53
Figure 26.54
Orbital Sarcoidosis
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 26.55
Figure 26.56
Figure 26.57
Figure 26.58
Figure 26.59
Figure 26.60
Orbital Granulomatosis with Polyangiitis (Wegener Granulomatosis)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 26.61
Figure 26.62
Figure 26.63
Figure 26.64
Figure 26.65
Figure 26.66
Kimura Disease and Angiolymphoid Hyperplasia with Eosinophilia
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Angiolymphoid Hyperplasia with Eosinophilia and Kimura Disease
Figure 26.67
Figure 26.68
Figure 26.69
Figure 26.70
Figure 26.71
Figure 26.72
Chapter 27: Orbital Cystic Lesions
Orbital Dermoid Cyst
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Dermoid Cyst: Typical Case of Epidermal Origin
Figure 27.1
Figure 27.2
Figure 27.3
Figure 27.4
Figure 27.5
Figure 27.6
Orbital Dermoid Cyst: Lesion of Conjunctival Origin in a Child
Figure 27.7
Figure 27.8
Figure 27.9
Figure 27.10
Figure 27.11
Figure 27.12
Orbital Dermoid Cyst: Lesion of Conjunctival Origin in an Adult
Figure 27.13
Figure 27.14
Figure 27.15
Figure 27.16
Figure 27.17
Figure 27.18
Orbital Dermoid Cyst: Dumbbell Type
Figure 27.19
Figure 27.20
Figure 27.21
Figure 27.22
Figure 27.23
Figure 27.24
Orbital Dermoid Cyst: Dumbbell Type, Surgical Resection
Figure 27.25
Figure 27.26
Figure 27.27
Figure 27.28
Figure 27.29
Figure 27.30
Orbital Dermoid Cyst: Deep Orbital Type
Figure 27.31
Figure 27.32
Figure 27.33
Figure 27.34
Figure 27.35
Figure 27.36
Orbital Simple Primary Cyst of Conjunctival Origin
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Orbital Cyst of Conjunctival Origin: Primary Idiopathic Type
Figure 27.37
Figure 27.38
Figure 27.39
Figure 27.40
Figure 27.41
Figure 27.42
Orbital Cyst of Conjunctival Origin: Secondary Type, after Enucleation
Figure 27.43
Figure 27.44
Figure 27.45
Figure 27.46
Figure 27.47
Figure 27.48
Orbital Cyst of Conjunctival Origin: Secondary Type, after Retinal Detachment Surgery
Figure 27.49
Figure 27.50
Figure 27.51
Figure 27.52
Figure 27.53
Figure 27.54
Orbital Cyst: Simple Conjunctival Type Associated with Stevens–Johnson Syndrome
Figure 27.55
Figure 27.56
Figure 27.57
Figure 27.58
Figure 27.59
Figure 27.60
Orbital Teratoma (Teratomatous Cyst)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Orbital Teratoma (Teratomatous Cyst) Discovered in Utero
Figure 27.61
Figure 27.62
Figure 27.63
Figure 27.64
Figure 27.65
Figure 27.66
Orbital Teratoma (Teratomatous Cyst)
Figure 27.67
Figure 27.68
Figure 27.69
Figure 27.70
Figure 27.71
Figure 27.72
Orbital Congenital Cystic Eye
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Orbital Congenital Cystic Eye Discovered in Utero
Figure 27.73
Figure 27.74
Figure 27.75
Figure 27.76
Figure 27.77
Figure 27.78
Orbital Colobomatous Cyst (Microphthalmos with Cyst)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Orbital Colobomatous Cyst
Figure 27.79
Figure 27.80
Figure 27.81
Figure 27.82
Figure 27.83
Figure 27.84
Orbital Colobomatous Cyst: Bilateral Occurrence, Clinicopathologic Correlation
Figure 27.85
Figure 27.86
Figure 27.87
Figure 27.88
Figure 27.89
Figure 27.90
Orbital Colobomatous Cyst: Clinical Variations, Ultrasonography, and Pathology
Figure 27.91
Figure 27.92
Figure 27.93
Figure 27.94
Figure 27.95
Figure 27.96
Orbital Cephalocele
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Orbital Cephalocele: Anterior (Ethmoidal) Type
Figure 27.97
Figure 27.98
Figure 27.99
Figure 27.100
Figure 27.101
Figure 27.102
Orbital Cephalocele: Posterior (Sphenoidal) Type
Figure 27.103
Figure 27.104
Figure 27.105
Figure 27.106
Figure 27.107
Figure 27.108
Orbital Mucocele
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Figure 27.109
Figure 27.110
Figure 27.111
Figure 27.112
Figure 27.113
Figure 27.114
Orbital Mucocele: Clinical, Imaging, and Histopathologic Correlations
Figure 27.115
Figure 27.116
Figure 27.117
Figure 27.118
Figure 27.119
Figure 27.120
Orbital Respiratory Epithelial Cyst
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Figure 27.121
Figure 27.122
Figure 27.123
Figure 27.124
Figure 27.125
Figure 27.126
Orbital Parasitic Cysts
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Hydatid Cyst
Figure 27.127
Figure 27.128
Figure 27.129
Figure 27.130
Figure 27.131
Figure 27.132
Figure 27.133
Figure 27.134
Figure 27.135
Figure 27.136
Figure 27.137
Figure 27.138
Chapter 28: Orbital Vascular and Hemorrhagic Lesions
Orbital Capillary Hemangioma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Figure 28.1
Figure 28.2
Figure 28.3
Figure 28.4
Figure 28.5
Figure 28.6
Orbital Capillary Hemangioma: Clinical Variations and Regression
Figure 28.7
Figure 28.8
Figure 28.9
Figure 28.10
Figure 28.11
Figure 28.12
Orbital Capillary Hemangioma: Simultaneous Eyelid and Adnexal Involvement
Figure 28.13
Figure 28.14
Figure 28.15
Figure 28.16
Figure 28.17
Figure 28.18
Orbital Capillary Hemangioma: Surgical Resection
Figure 28.19
Figure 28.20
Figure 28.21
Figure 28.22
Figure 28.23
Figure 28.24
Orbital Cavernous Hemangioma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 28.25
Figure 28.26
Figure 28.27
Figure 28.28
Figure 28.29
Figure 28.30
Orbital Cavernous Hemangioma: Surgical Removal by Conjunctival Approach
Figure 28.31
Figure 28.32
Figure 28.33
Figure 28.34
Figure 28.35
Figure 28.36
Orbital Cavernous Hemangioma: Globe and Optic Nerve Compression
Figure 28.37
Figure 28.38
Figure 28.39
Figure 28.40
Figure 28.41
Figure 28.42
Orbital Cavernous Hemangioma: Clinicopathologic Correlation
Figure 28.43
Figure 28.44
Figure 28.45
Figure 28.46
Figure 28.47
Figure 28.48
Orbital Cavernous Hemangioma: Superonasal Orbitotomy
Figure 28.49
Figure 28.50
Figure 28.51
Figure 28.52
Figure 28.53
Figure 28.54
Orbital Cavernous Hemangioma: Intraosseous Type
Figure 28.55
Figure 28.56
Figure 28.57
Figure 28.58
Figure 28.59
Figure 28.60
Orbital Hemangiopericytoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Hemangiopericytoma: Clinicopathologic Correlation
Figure 28.61
Figure 28.62
Figure 28.63
Figure 28.64
Figure 28.65
Figure 28.66
Figure 28.67
Figure 28.68
Figure 28.69
Figure 28.70
Figure 28.71
Figure 28.72
Orbital Hemangiopericytoma: Aggressive Tumor with Brain Invasion
Figure 28.73
Figure 28.74
Figure 28.75
Figure 28.76
Figure 28.77
Figure 28.78
Orbital Lymphangioma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Lymphangioma: Clinical and Pathologic Features
Figure 28.79
Figure 28.80
Figure 28.81
Figure 28.82
Figure 28.83
Figure 28.84
Orbital Lymphangioma: CT and MRI
Figure 28.85
Figure 28.86
Figure 28.87
Figure 28.88
Figure 28.89
Figure 28.90
Orbital Lymphangioma: MRI Features and Management by Aspiration
Figure 28.91
Figure 28.92
Figure 28.93
Figure 28.94
Figure 28.95
Figure 28.96
Orbital Lymphangioma: Occurrence in an Infant
Figure 28.97
Figure 28.98
Figure 28.99
Figure 28.100
Figure 28.101
Figure 28.102
Orbital Lymphangioma: Occurrence in a Young Child
Figure 28.103
Figure 28.104
Figure 28.105
Figure 28.106
Figure 28.107
Figure 28.108
Orbital Lymphangioma: Occurrence in an Older Adult
Figure 28.109
Figure 28.110
Figure 28.111
Figure 28.112
Figure 28.113
Figure 28.114
Orbital Varix
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Varix: Demonstration by Increasing Intracranial Venous Pressure
Figure 28.115
Figure 28.116
Figure 28.117
Figure 28.118
Figure 28.119
Figure 28.120
Orbital Varix: Demonstration by Valsalva Maneuver
Figure 28.121
Figure 28.122
Figure 28.123
Figure 28.124
Figure 28.125
Figure 28.126
Orbital Varix: Computed Tomography, Magnetic Resonance Imaging, and Color Doppler Imaging
Figure 28.127
Figure 28.128
Figure 28.129
Figure 28.130
Figure 28.131
Figure 28.132
Orbital Varix: Anteriorly Located Lesion
Figure 28.133
Figure 28.134
Figure 28.135
Figure 28.136
Figure 28.137
Figure 28.138
Orbital Miscellaneous Vascular Lesions: Intravascular Papillary Endothelial Hyperplasia and Glomus Tumor of the Orbit
Orbital Intravascular Papillary Endothelial Hyperplasia
General Considerations
Clinical Features
Pathology and Pathogenesis
Diagnostic Approaches
Management
Selected References
Orbital Intravascular Papillary Endothelial Hyperplasia and Glomus Tumor
Figure 28.139
Figure 28.140
Figure 28.141
Figure 28.142
Figure 28.143
Figure 28.144
Orbital Angiosarcoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 28.145
Figure 28.146
Figure 28.147
Figure 28.148
Figure 28.149
Figure 28.150
Orbital Hematoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Organizing Hematoma
Figure 28.151
Figure 28.152
Figure 28.153
Figure 28.154
Figure 28.155
Figure 28.156
Chapter 29: Orbital Peripheral Nerve Tumors
Orbital (Neurilemoma)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Schwannoma
Figure 29.1
Figure 29.2
Figure 29.3
Figure 29.4
Figure 29.5
Figure 29.6
Figure 29.7
Figure 29.8
Figure 29.9
Figure 29.10
Figure 29.11
Figure 29.12
Figure 29.13
Figure 29.14
Figure 29.15
Figure 29.16
Figure 29.17
Figure 29.18
Orbital Schwannoma: Intracranial Extension
Figure 29.19
Figure 29.20
Figure 29.21
Figure 29.22
Figure 29.23
Figure 29.24
Orbital Neurofibroma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Neurofibroma: Association with Neurofibromatosis
Figure 29.25
Figure 29.26
Figure 29.27
Figure 29.28
Figure 29.29
Figure 29.30
Orbital Neurofibroma: Progression of Eyelid, Orbital, and Intraocular Neurofibromatosis
Figure 29.31
Figure 29.32
Figure 29.33
Figure 29.34
Figure 29.35
Figure 29.36
Orbital Neurofibroma: Solitary Type Unassociated with Neurofibromatosis
Figure 29.37
Figure 29.38
Figure 29.39
Figure 29.40
Figure 29.41
Figure 29.42
Orbital Neurofibroma: Multiple Circumscribed Type Unassociated with Neurofibromatosis
Figure 29.43
Figure 29.44
Figure 29.45
Figure 29.46
Figure 29.47
Figure 29.48
Orbital Paraganglioma (Chemodectoma)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Prognosis
Selected References
Orbital Paraganglioma
Figure 29.49
Figure 29.50
Figure 29.51
Figure 29.52
Figure 29.53
Figure 29.54
Orbital Alveolar Soft Part Sarcoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 29.55
Figure 29.56
Figure 29.57
Figure 29.58
Figure 29.59
Figure 29.60
Orbital Alveolar Soft Part Sarcoma: Aggressive Tumor in a Child
Figure 29.61
Figure 29.62
Figure 29.63
Figure 29.64
Figure 29.65
Figure 29.66
Miscellaneous Orbital Neural Tumors: Granular Cell Tumor, Amputation Neuroma, and Malignant Peripheral Nerve Sheath Tumor
Orbital Granular Cell Tumor
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Orbital Amputation Neuroma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management and Prognosis
Selected References
Orbital Malignant Peripheral Nerve Sheath Tumor
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management and Prognosis
Selected References
Orbital Miscellaneous Neural Tumors: Granular Cell Tumor, Amputation Neuroma, and Malignant Peripheral Nerve Sheath Tumor
Figure 29.67
Figure 29.68
Figure 29.69
Figure 29.70
Figure 29.71
Figure 29.72
Chapter 30: Optic Nerve, Meningeal, and Other Neural Tumors
Optic Nerve Juvenile Pilocytic Astrocytoma (Optic Nerve Glioma): General Considerations
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management and Prognosis
Selected References
Optic Nerve Juvenile Pilocytic Astrocytoma (Glioma)
Figure 30.1
Figure 30.2
Figure 30.3
Figure 30.4
Figure 30.5
Figure 30.6
Optic Nerve Juvenile Pilocytic Astrocytoma (Glioma): Magnetic Resonance Imaging
Figure 30.7
Figure 30.8
Figure 30.9
Figure 30.10
Figure 30.11
Figure 30.12
Optic Nerve Juvenile Pilocytic Astrocytoma (Glioma)
Figure 30.13
Figure 30.14
Figure 30.15
Figure 30.16
Figure 30.17
Figure 30.18
Optic Nerve Juvenile Pilocytic Astrocytoma (Glioma): Fundus Changes
Figure 30.19
Figure 30.20
Figure 30.21
Figure 30.22
Figure 30.23
Figure 30.24
Optic Nerve Malignant Astrocytoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 30.25
Figure 30.26
Figure 30.27
Figure 30.28
Figure 30.29
Figure 30.30
Optic Nerve Sheath Meningioma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 30.31
Figure 30.32
Figure 30.33
Figure 30.34
Figure 30.35
Figure 30.36
Optic Nerve Sheath Meningioma: Magnetic Resonance Imaging
Figure 30.37
Figure 30.38
Figure 30.39
Figure 30.40
Figure 30.41
Figure 30.42
Optic Nerve Sheath Meningioma: Aggressive Variant
Figure 30.43
Figure 30.44
Figure 30.45
Figure 30.46
Figure 30.47
Figure 30.48
Orbital Sphenoid Wing Meningioma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Sphenoid Wing Meningioma: Orbital Involvement
Figure 30.49
Figure 30.50
Figure 30.51
Figure 30.52
Figure 30.53
Figure 30.54
Figure 30.55
Figure 30.56
Figure 30.57
Figure 30.58
Figure 30.59
Figure 30.60
Orbital Primitive Neuroectodermal Tumor and Primary Orbital Neuroblastoma
Orbital Primitive Neuroectodermal Tumor
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Neuroblastoma: Primary Type
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 30.61
Figure 30.62
Figure 30.63
Figure 30.64
Figure 30.65
Figure 30.66
Chapter 31: Orbital Myogenic Tumors
Orbital Rhabdomyosarcoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Prognosis
Selected References
Table 31.1: Intergroup Rhabdomyosarcoma Study Group Staging Classification
Figure 31.1
Figure 31.2
Figure 31.3
Figure 31.4
Figure 31.5
Figure 31.6
Orbital Rhabdomyosarcoma Simulating a Lymphangioma
Figure 31.7
Figure 31.8
Figure 31.9
Figure 31.10
Figure 31.11
Figure 31.12
Orbital Rhabdomyosarcoma: Typical Case—clinical Features, MRI, and Pathology
Figure 31.13
Figure 31.14
Figure 31.15
Figure 31.16
Figure 31.17
Figure 31.18
Orbital Rhabdomyosarcoma: Presentation as a Conjunctival Mass
Figure 31.19
Figure 31.20
Figure 31.21
Figure 31.22
Figure 31.23
Figure 31.24
Orbital Rhabdomyosarcoma: Biopsy Approach
Figure 31.25
Figure 31.26
Figure 31.27
Figure 31.28
Figure 31.29
Figure 31.30
Orbital Rhabdomyosarcoma: Simulating Orbital Hematoma in a Child
Figure 31.31
Figure 31.32
Figure 31.33
Figure 31.34
Figure 31.35
Figure 31.36
Orbital Rhabdomyosarcoma: Advanced Aggressive Cases
Figure 31.37
Figure 31.38
Figure 31.39
Figure 31.40
Figure 31.41
Figure 31.42
Orbital Malignant Rhabdoid Tumor
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 31.43
Figure 31.44
Figure 31.45
Figure 31.46
Figure 31.47
Figure 31.48
Orbital Leiomyoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Leiomyosarcoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Leiomyoma and Leiomyosarcoma
Figure 31.49
Figure 31.50
Figure 31.51
Figure 31.52
Figure 31.53
Figure 31.54
Chapter 32: Orbital Fibrous Connective Tissue Tumors
Orbital Nodular Fasciitis and Fibroma
Orbital Nodular Fasciitis
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Fibroma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Nodular Fasciitis
Figure 32.1
Figure 32.2
Figure 32.3
Figure 32.4
Figure 32.5
Figure 32.6
Orbital Nodular Fasciitis and Fibroma
Figure 32.7
Figure 32.8
Figure 32.9
Figure 32.10
Figure 32.11
Figure 32.12
Orbital Fibromatosis, Myofibromatosis, and Myofibroma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Infantile Fibromatosis
Figure 32.13
Figure 32.14
Figure 32.15
Figure 32.16
Figure 32.17
Figure 32.18
Orbital Infantile Myofibromatosis
Figure 32.19
Figure 32.20
Figure 32.21
Figure 32.22
Figure 32.23
Figure 32.24
Orbital Fibrous Histiocytoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Fibrous Histiocytoma: Benign Type
Figure 32.25
Figure 32.26
Figure 32.27
Figure 32.28
Figure 32.29
Figure 32.30
Orbital Fibrous Histiocytoma: Malignant Type
Figure 32.31
Figure 32.32
Figure 32.33
Figure 32.34
Figure 32.35
Figure 32.36
Orbital Fibrous Histiocytoma: Management
Figure 32.37
Figure 32.38
Figure 32.39
Figure 32.40
Figure 32.41
Figure 32.42
Orbital Solitary Fibrous Tumor
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 32.43
Figure 32.44
Figure 32.45
Figure 32.46
Figure 32.47
Figure 32.48
Orbital Solitary Fibrous Tumor with Slow-Onset Recurrence
Figure 32.49
Figure 32.50
Figure 32.51
Figure 32.52
Figure 32.53
Figure 32.54
Orbital Fibrosarcoma
Selected References
Figure 32.55
Figure 32.56
Figure 32.57
Figure 32.58
Figure 32.59
Figure 32.60
Chapter 33: Orbital Osseous, Fibro-Osseous, and Cartilaginous Tumors
Orbital Osteoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 33.1
Figure 33.2
Figure 33.3
Figure 33.4
Figure 33.5
Figure 33.6
Orbital Osteoma: Clinicopathologic and Imaging Correlation and Occurrence in Gardner’s Syndrome
Figure 33.7
Figure 33.8
Figure 33.9
Figure 33.10
Figure 33.11
Figure 33.12
Orbit Osteosarcoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Orbital Osteosarcoma
Figure 33.13
Figure 33.14
Figure 33.15
Figure 33.16
Figure 33.17
Figure 33.18
Orbital Fibrous Dysplasia
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 33.19
Figure 33.20
Figure 33.21
Figure 33.22
Figure 33.23
Figure 33.24
Figure 33.25
Figure 33.26
Figure 33.27
Figure 33.28
Figure 33.29
Figure 33.30
Orbital Ossifying Fibroma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 33.31
Figure 33.32
Figure 33.33
Figure 33.34
Figure 33.35
Figure 33.36
Figure 33.37
Figure 33.38
Figure 33.39
Figure 33.40
Figure 33.41
Figure 33.42
Orbital Giant Cell Reparative Granuloma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 33.43
Figure 33.44
Figure 33.45
Figure 33.46
Figure 33.47
Figure 33.48
Orbital Cartilaginous Chondroma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Chondroma
Figure 33.49
Figure 33.50
Figure 33.51
Figure 33.52
Figure 33.53
Figure 33.54
Orbital Chondrosarcoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 33.55
Figure 33.56
Figure 33.57
Figure 33.58
Figure 33.59
Figure 33.60
Orbital Chondrosarcoma in a Young Woman
Figure 33.61
Figure 33.62
Figure 33.63
Figure 33.64
Figure 33.65
Figure 33.66
Chapter 34: Orbital Lipomatous and Myxomatous Tumors
Orbital Fat Prolapse
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 34.1
Figure 34.2
Figure 34.3
Figure 34.4
Figure 34.5
Figure 34.6
Figure 34.7
Figure 34.8
Figure 34.9
Figure 34.10
Figure 34.11
Figure 34.12
Orbital Fat Prolapse: Clinical and Computed Tomography Features and Surgical Approach
Figure 34.13
Figure 34.14
Figure 34.15
Figure 34.16
Figure 34.17
Figure 34.18
Orbital/Conjunctival Dermolipoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology and Pathogenesis
Management
Selected References
Orbital/Conjunctival Dermolipoma: Clinical Spectrum and Age Range
Figure 34.19
Figure 34.20
Figure 34.21
Figure 34.22
Figure 34.23
Figure 34.24
Orbital/Conjunctival Dermolipoma: Clinical, Computed Tomography, and Histopathologic Features
Figure 34.25
Figure 34.26
Figure 34.27
Figure 34.28
Figure 34.29
Figure 34.30
Orbital/Conjunctival Dermolipoma: Association with Goldenhar Syndrome
Figure 34.31
Figure 34.32
Figure 34.33
Figure 34.34
Figure 34.35
Figure 34.36
Orbital Lipoma and Myxoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Pleomorphic Lipoma: Clinical, Magnetic Resonance Imaging, and Histopathologic Findings
Figure 34.37
Figure 34.38
Figure 34.39
Figure 34.40
Figure 34.41
Figure 34.42
Orbital Lipoma: Clinicopathologic Variations
Figure 34.43
Figure 34.44
Figure 34.45
Figure 34.46
Figure 34.47
Figure 34.48
Orbital Myxoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 34.49
Figure 34.50
Figure 34.51
Figure 34.52
Figure 34.53
Figure 34.54
Orbital Liposarcoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 34.55
Figure 34.56
Figure 34.57
Figure 34.58
Figure 34.59
Figure 34.60
Chapter 35: Orbital Histiocytic Tumors
Orbit Juvenile Xanthogranuloma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Juvenile Xanthogranuloma
Figure 35.1
Figure 35.2
Figure 35.3
Figure 35.4
Figure 35.5
Figure 35.6
Orbital Adult-Onset Xanthogranuloma with Asthma
Figure 35.7
Figure 35.8
Figure 35.9
Figure 35.10
Figure 35.11
Figure 35.12
Orbital Langerhans’ Cell Histiocytosis (Eosinophilic Granuloma)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Langerhans’ Cell Histiocytosis (Eosinophilic Granuloma): Clinical, Computed Tomography, and Pathologic Features
Figure 35.13
Figure 35.14
Figure 35.15
Figure 35.16
Figure 35.17
Figure 35.18
Orbital Langerhans’ Cell Histiocytosis (Eosinophilic Granuloma): Bilateral Sequential Orbital Involvement
Figure 35.19
Figure 35.20
Figure 35.21
Figure 35.22
Figure 35.23
Figure 35.24
Orbital Langerhans’ Cell Histiocytosis (Eosinophilic Granuloma): Management
Figure 35.25
Figure 35.26
Figure 35.27
Figure 35.28
Figure 35.29
Figure 35.30
Orbital Langerhans’ Cell Histiocytosis (Eosinophilic Granuloma): Presentation as a Hemorrhagic, Cystic Lesion
Figure 35.31
Figure 35.32
Figure 35.33
Figure 35.34
Figure 35.35
Figure 35.36
Orbital Erdheim–Chester Disease
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 35.37
Figure 35.38
Figure 35.39
Figure 35.40
Figure 35.41
Figure 35.42
Orbital Rosai–Dorfman Disease (Sinus Histiocytosis with Massive Lymphadenopathy)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 35.43
Figure 35.44
Figure 35.45
Figure 35.46
Figure 35.47
Figure 35.48
Necrobiotic Xanthogranuloma and Multinucleate Cell Angiohistiocytoma
Orbital Necrobiotic Xanthogranuloma
General Considerations
Clinical Features
Pathology
Management
Selected References
Orbital Multinucleate Cell Angiohistiocytoma
General Considerations
Clinical Features
Pathology
Diagnostic Approaches
Selected References
Orbital Necrobiotic Xanthogranuloma and Multinucleate Cell Angiohistiocytoma
Figure 35.49
Figure 35.50
Figure 35.51
Figure 35.52
Figure 35.53
Figure 35.54
Chapter 36: Orbital Primary Melanocytic Tumors
Orbital Melanoma Arising from Ocular Melanocytosis and Blue Nevus
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Melanoma Arising from Blue Nevus
Figure 36.1
Figure 36.2
Figure 36.3
Figure 36.4
Figure 36.5
Figure 36.6
Orbital Melanomas Arising De Novo
General Considerations
Clinical Features
Diagnostic Approaches
Management and Prognosis
Selected References
Orbital Melanoma: De Novo Primary Tumors
Figure 36.7
Figure 36.8
Figure 36.9
Figure 36.10
Figure 36.11
Figure 36.12
Orbital Melanocytic Hamartoma and Melanotic Neuroectodermal Tumor
Orbital Melanocytic Hamartoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Orbital Involvement by Melanotic Neuroectodermal Tumor
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Melanocytic Hamartoma and Melanotic Neuroectodermal Tumor
Figure 36.13
Figure 36.14
Figure 36.15
Figure 36.16
Figure 36.17
Figure 36.18
Chapter 37: Lacrimal Gland Primary Epithelial Tumors
Introduction: Lacrimal Gland Lesions
General References
Lacrimal Gland Ductal Epithelial Cyst (Dacryops)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 37.1
Figure 37.2
Figure 37.3
Figure 37.4
Figure 37.5
Figure 37.6
Figure 37.7
Figure 37.8
Figure 37.9
Figure 37.10
Figure 37.11
Figure 37.12
Lacrimal Gland Pleomorphic Adenoma (Benign Mixed Tumor)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Lacrimal Gland Pleomorphic Adenoma: Clinicopathologic Correlation
Figure 37.13
Figure 37.14
Figure 37.15
Figure 37.16
Figure 37.17
Figure 37.18
Lacrimal Gland Pleomorphic Adenoma: Surgical Management
Figure 37.19
Figure 37.20
Figure 37.21
Figure 37.22
Figure 37.23
Figure 37.24
Lacrimal Gland Pleomorphic Adenoma in a Teenager
Figure 37.25
Figure 37.26
Figure 37.27
Figure 37.28
Figure 37.29
Figure 37.30
Lacrimal Gland Pleomorphic Adenoma: Magnetic Resonance Imaging
Figure 37.31
Figure 37.32
Figure 37.33
Figure 37.34
Figure 37.35
Figure 37.36
Lacrimal Gland Pleomorphic Adenocarcinoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Lacrimal Gland Pleomorphic Adenocarcinoma (Malignant Mixed Tumor)
Figure 37.37
Figure 37.38
Figure 37.39
Figure 37.40
Figure 37.41
Figure 37.42
Lacrimal Gland Adenoid Cystic Carcinoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 37.43
Figure 37.44
Figure 37.45
Figure 37.46
Figure 37.47
Figure 37.48
Lacrimal Gland Adenoid Cystic Carcinoma: Clinicopathologic Correlation of an Aggressive Case
Figure 37.49
Figure 37.50
Figure 37.51
Figure 37.52
Figure 37.53
Figure 37.54
Lacrimal Gland Adenoid Cystic Carcinoma: Early Detection by Imaging Studies and Treatment with Brachytherapy
Figure 37.55
Figure 37.56
Figure 37.57
Figure 37.58
Figure 37.59
Figure 37.60
Lacrimal Gland Adenoid Cystic Carcinoma: Occurrence in a Child
Figure 37.61
Figure 37.62
Figure 37.63
Figure 37.64
Figure 37.65
Figure 37.66
Lacrimal Gland Adenoid Cystic Carcinoma: Atypical Nasal Orbital Location
Figure 37.67
Figure 37.68
Figure 37.69
Figure 37.70
Figure 37.71
Figure 37.72
Lacrimal Gland Primary Ductal Carcinoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 37.73
Figure 37.74
Figure 37.75
Figure 37.76
Figure 37.77
Figure 37.78
Lacrimal Gland Mucoepidermoid Carcinoma
Figure 37.79
Figure 37.80
Figure 37.81
Figure 37.82
Figure 37.83
Figure 37.84
Histopathology of Primary Epithelial Malignancies of Lacrimal Gland
Adenoid Cystic Carcinoma
Pleomorphic Adenocarcinoma
Primary Adenocarcinoma
Mucoepidermoid Carcinoma
Primary Squamous Cell Carcinoma
Sebaceous Carcinoma
Acinic Cell Adenocarcinoma
Ductal Carcinoma
Lymphoepithelial Carcinoma
Basal Cell Adenocarcinoma
Epithelial–Myoepithelial Carcinoma
Cystadenocarcinoma
Selected References
Lacrimal Gland: Histopathology of Selected Primary Epithelial Malignancies
Figure 37.85
Figure 37.86
Figure 37.87
Figure 37.88
Figure 37.89
Figure 37.90
Chapter 38: Orbital Metastatic Cancer
Orbital Metastatic Cancer
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Metastasis from Breast Cancer
Figure 38.1
Figure 38.2
Figure 38.3
Figure 38.4
Figure 38.5
Figure 38.6
Orbital Metastasis from Breast Cancer: Clinical Variations
Figure 38.7
Figure 38.8
Figure 38.9
Figure 38.10
Figure 38.11
Figure 38.12
Orbital Metastasis from Breast Cancer: Paradoxical Enophthalmos
Figure 38.13
Figure 38.14
Figure 38.15
Figure 38.16
Figure 38.17
Figure 38.18
Orbital Metastasis from Breast Cancer: Biopsy Techniques
Figure 38.19
Figure 38.20
Figure 38.21
Figure 38.22
Figure 38.23
Figure 38.24
Orbital Metastasis from Prostate Carcinoma
Figure 38.25
Figure 38.26
Figure 38.27
Figure 38.28
Figure 38.29
Figure 38.30
Orbital Metastasis from Carcinoid Tumor
Figure 38.31
Figure 38.32
Figure 38.33
Figure 38.34
Figure 38.35
Figure 38.36
Orbital Metastasis from Lung Cancer
Figure 38.37
Figure 38.38
Figure 38.39
Figure 38.40
Figure 38.41
Figure 38.42
Orbital Metastasis from Renal Cell Carcinoma
Figure 38.43
Figure 38.44
Figure 38.45
Figure 38.46
Figure 38.47
Figure 38.48
Orbital Metastasis from Cutaneous Melanoma
Figure 38.49
Figure 38.50
Figure 38.51
Figure 38.52
Figure 38.53
Figure 38.54
Orbital Metastasis from Choroidal Melanoma
Figure 38.55
Figure 38.56
Figure 38.57
Figure 38.58
Figure 38.59
Figure 38.60
Orbital Metastasis from Choroidal Melanoma to the Contralateral Orbit
Figure 38.61
Figure 38.62
Figure 38.63
Figure 38.64
Figure 38.65
Figure 38.66
Orbital Metastasis from Thyroid Cancer and Orbital Metastasis from an Unknown Primary Site
Figure 38.67
Figure 38.68
Figure 38.69
Figure 38.70
Figure 38.71
Figure 38.72
Orbital Metastasis of Adrenal Neuroblastoma
Figure 38.73
Figure 38.74
Figure 38.75
Figure 38.76
Figure 38.77
Figure 38.78
Orbital Metastasis: Wilms’ Tumor, Ewing’s Tumor, and Rhabdomyosarcoma
Figure 38.79
Figure 38.80
Figure 38.81
Figure 38.82
Figure 38.83
Figure 38.84
Chapter 39: Orbital Lymphoid Tumors and Leukemias
Orbital Non-Hodgkin Lymphoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Table 39.1: World Health Organization (WHO) 2008 classification of B-cell neoplasms
Table 39.2: American Joint Committee on Cancer (AJCC) classification of ocular adnexal lymphoma
Orbital Non-Hodgkin Lymphoma: Clinical, Computed Tomography, and Magnetic Resonance Imaging Features
Figure 39.1
Figure 39.2
Figure 39.3
Figure 39.4
Figure 39.5
Figure 39.6
Orbital Non-Hodgkin Lymphoma: Clinical Variations and Pathology
Figure 39.7
Figure 39.8
Figure 39.9
Figure 39.10
Figure 39.11
Figure 39.12
Orbital Lacrimal Gland Lymphoma: Clinical and Magnetic Resonance Imaging Correlations
Figure 39.13
Figure 39.14
Figure 39.15
Figure 39.16
Figure 39.17
Figure 39.18
Orbital Non-Hodgkin Lymphoma: Diagnosis and Management
Figure 39.19
Figure 39.20
Figure 39.21
Figure 39.22
Figure 39.23
Figure 39.24
Orbital Lymphoma: Atypical Forms
Selected References
Orbital Lymphoma: Atypical Forms: Large Cell Lymphoma with Microvillous Projections and Cutaneous T-Cell Lymphoma
Figure 39.25
Figure 39.26
Figure 39.27
Figure 39.28
Figure 39.29
Figure 39.30
Orbital Plasmacytoma and Lymphoplasmacytoid Tumors
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 39.31
Figure 39.32
Figure 39.33
Figure 39.34
Figure 39.35
Figure 39.36
Orbital Plasmacytoma: Association with Multiple Myeloma
Figure 39.37
Figure 39.38
Figure 39.39
Figure 39.40
Figure 39.41
Figure 39.42
Orbital Plasmablastic Lymphoma
General Consideration
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 39.43
Figure 39.44
Figure 39.45
Figure 39.46
Figure 39.47
Figure 39.48
Orbital Burkitt Lymphoma
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Figure 39.49
Figure 39.50
Figure 39.51
Figure 39.52
Figure 39.53
Figure 39.54
Orbital Post-Transplant Lymphoproliferative Disorder
General Considerations
Clinical Features
Pathology
Management
Selected References
Figure 39.55
Figure 39.56
Figure 39.57
Figure 39.58
Figure 39.59
Figure 39.60
Figure 39.61
Figure 39.62
Figure 39.63
Figure 39.64
Figure 39.65
Figure 39.66
Orbital–Orbital Involvement by Leukemia (Myeloid Sarcoma)
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Myeloid Sarcoma (Leukemia)
Figure 39.67
Figure 39.68
Figure 39.69
Figure 39.70
Figure 39.71
Figure 39.72
Orbital Myeloid Sarcoma (Leukemia): Bilateral Orbital Involvement
Figure 39.73
Figure 39.74
Figure 39.75
Figure 39.76
Figure 39.77
Figure 39.78
Chapter 40: Orbital Secondary Tumors
Orbital Secondary Tumors
General Considerations
Clinical Features
Diagnostic Approaches
Pathology
Management
Selected References
Orbital Invasion from Eyelid Basal Cell Carcinoma
Figure 40.1
Figure 40.2
Figure 40.3
Figure 40.4
Figure 40.5
Figure 40.6
Orbital Invasion from Eyelid Sebaceous Carcinoma: Simulating a Primary Lacrimal Gland Tumor
Figure 40.7
Figure 40.8
Figure 40.9
Figure 40.10
Figure 40.11
Figure 40.12
Orbital Invasion from Eyelid Melanoma
Figure 40.13
Figure 40.14
Figure 40.15
Figure 40.16
Figure 40.17
Figure 40.18
Orbital Invasion from Conjunctival Squamous Cell Carcinoma
Figure 40.19
Figure 40.20
Figure 40.21
Figure 40.22
Figure 40.23
Figure 40.24
Orbital Invasion from Conjunctival Melanoma
Figure 40.25
Figure 40.26
Figure 40.27
Figure 40.28
Figure 40.29
Figure 40.30
Orbital Invasion from Conjunctival Melanoma in a Young African American
Figure 40.31
Figure 40.32
Figure 40.33
Figure 40.34
Figure 40.35
Figure 40.36
Orbital Invasion from Uveal Melanoma: Massive Orbital Involvement
Figure 40.37
Figure 40.38
Figure 40.39
Figure 40.40
Figure 40.41
Figure 40.42
Orbital Invasion from Massive Choroidal Melanoma
Figure 40.43
Figure 40.44
Figure 40.45
Figure 40.46
Figure 40.47
Figure 40.48
Orbital Invasion from Retinoblastoma
Figure 40.49
Figure 40.50
Figure 40.51
Figure 40.52
Figure 40.53
Figure 40.54
Orbital Invasion from Massive Unrecognized Retinoblastoma
Figure 40.55
Figure 40.56
Figure 40.57
Figure 40.58
Figure 40.59
Figure 40.60
Orbital Invasion from Paranasal Sinus Cancers
Figure 40.61
Figure 40.62
Figure 40.63
Figure 40.64
Figure 40.65
Figure 40.66
Orbital Invasion from Nasopharyngeal Cancers
Figure 40.67
Figure 40.68
Figure 40.69
Figure 40.70
Figure 40.71
Figure 40.72
Chapter 41: Surgical Management of Orbital Tumors
Surgical Management of Orbital Tumors
Fine-Needle Aspiration Biopsy
Conjunctival Approach
Cutaneous Approach
Orbital Exenteration
Selected References
Orbital Surgery: Instrumentation and Conjunctival Approach
Figure 41.1
Figure 41.2
Figure 41.3
Figure 41.4
Figure 41.5
Figure 41.6
Orbital Surgery: Cutaneous Superonasal Approach
Figure 41.7
Figure 41.8
Figure 41.9
Figure 41.10
Figure 41.11
Figure 41.12
Orbital Surgery: Cutaneous Superotemporal Approach
Figure 41.13
Figure 41.14
Figure 41.15
Figure 41.16
Figure 41.17
Figure 41.18
Orbital Surgery: Cutaneous Superotemporal Approach
Figure 41.19
Figure 41.20
Figure 41.21
Figure 41.22
Figure 41.23
Figure 41.24
Orbital Surgery: Exenteration
Figure 41.25
Figure 41.26
Figure 41.27
Figure 41.28
Figure 41.29
Figure 41.30
Orbital Exenteration Prostheses
Figure 41.31
Figure 41.32
Figure 41.33
Figure 41.34
Figure 41.35
Figure 41.36
Orbital Exenteration: Cosmetic Rehabilitation
Figure 41.37
Figure 41.38
Figure 41.39
Figure 41.40
Figure 41.41
Figure 41.42
Appendix
Remarks
| An aparitie | 17 Oct. 2015 |
| Autor | Dr. Jerry A. Shields , Dr. Carol L. Shields |
| Dimensiuni | 213 x 276 x 40 mm |
| Editura | LWW |
| Format | Hardcover |
| ISBN | 9781496321480 |
| Limba | Engleza |
| Nr pag | 824 |
| Versiune digitala | DA |

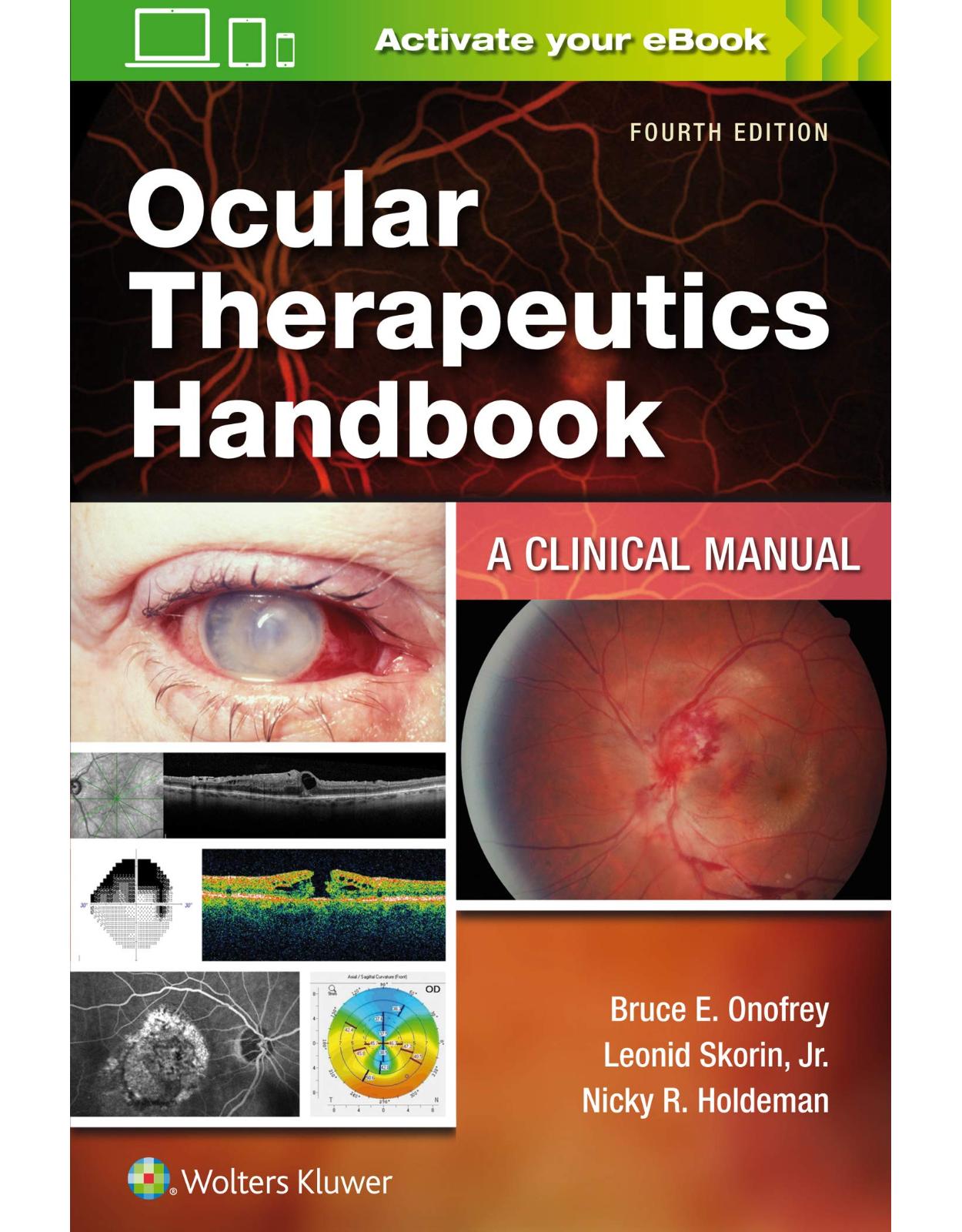
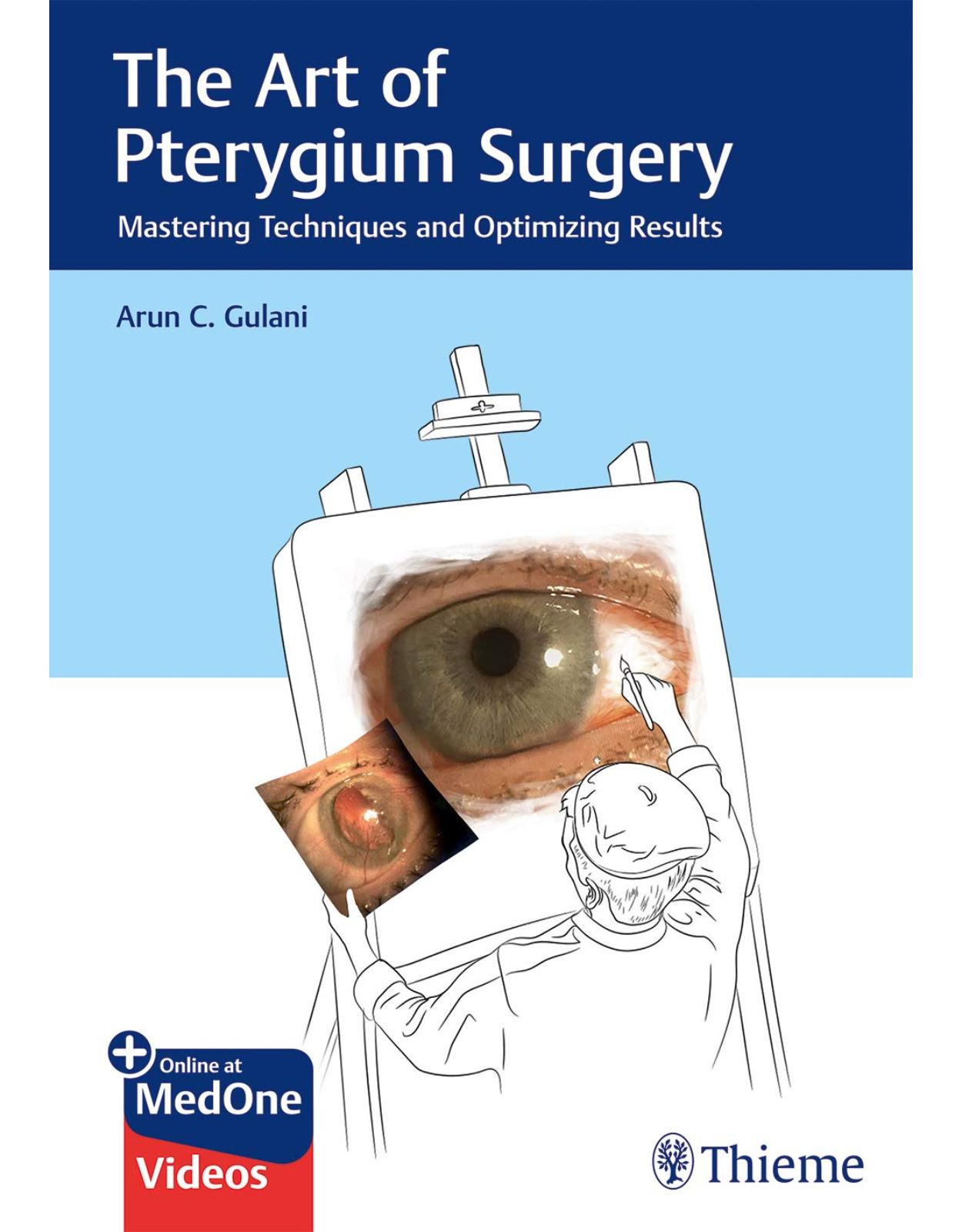
Clientii ebookshop.ro nu au adaugat inca opinii pentru acest produs. Fii primul care adauga o parere, folosind formularul de mai jos.