Lymphedema Management
Livrare gratis la comenzi peste 500 RON. Pentru celelalte comenzi livrarea este 20 RON.
Disponibilitate: La comanda in aproximativ 4-6 saptamani
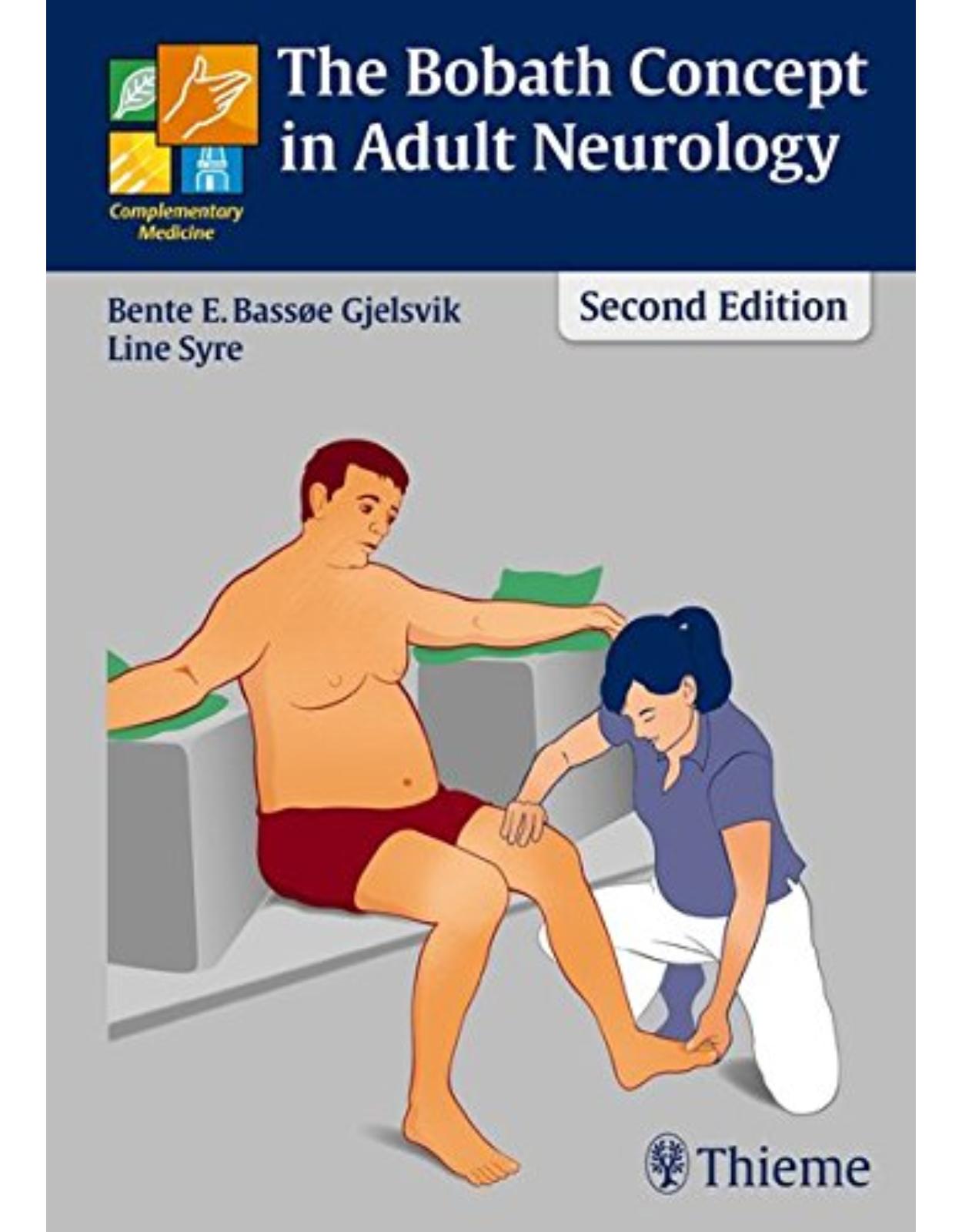
Editura: Thieme
Limba: Engleza
Nr. pagini: 600
Coperta: Hardback
Dimensiuni: 18.3 x 3 x 25.9 cm
An aparitie: 2017
Description:
FIVE STARS from Doody's Star Ratings™
This essential guide encompasses the core principles of Manual Lymph Drainage and Complete Decongestive Therapy for a wide range of pathologies across the age continuum. Key elements from the prior edition are incorporated, such as color-coded sections for anatomy, physiology, and pathophysiology. Advances in the field are reflected in expanded chapters and efficacy meta-analyses, updates on genetics, refinements in manual compression, and new insights on fat disorders and edema.
Key highlights in fourth edition
More than 140 new color images, over 30 new tables, and updated ICD-10 codes
Expanded discussion of lipedema and related conditions such as Dercum's and Madelung's diseases
Surgical approaches such as vascularized lymph node transfer, anastomosis and bypass techniques, suction assisted protein lipectomy, and combined and staged lymphedema operations
Wound care options for edema and advanced venous disease
Integration of conventional therapies and techniques in collaboration with surgeons who perform specialized lymphatic procedures
Tips and guidance for growing numbers of home care focused practitioners who encounter lymphedema and related edemas in patients
Management of garments including fit, functionality, and patient independence
Rare pediatric syndromes and adaption of CDT for children
Expanded discussion of sequential intermittent pneumatic compression including contraindications and usages in lymphedema management
This is a must-have resource on the diagnosis, treatment, and management of lymphedema and lymphatic insufficiency. Its unique practicality will enable educators to teach techniques and clinicians to adeptly incorporate a wide range of treatment strategies into practice.
Table of Contents:
1 Anatomy
1.1 Circulatory System
1.1.1 Components
1.1.2 Systemic Circulation
1.2 Lymphatic System
1.2.1 Function
1.2.2 Components of the Lymphatic System
1.2.3 Embryology and Development of the Lymphatic System
1.3 Topography of the Lymphatic System
1.3.1 Lymph Fluid
1.3.2 Lymphatic Loads
1.3.3 Lymphatic Vessels
1.3.4 Lymphatic Tissues
1.4 Lymphatic Watersheds
1.4.1 Sagittal Watershed
1.4.2 Horizontal Watershed
1.4.3 Watersheds between the Trunk and the Extremities
1.5 Interterritorial Anastomoses
1.5.1 Anterior Axillo-axillary (AAA) Anastomosis
1.5.2 Posterior Axillo-axillary (PAA) Anastomosis
1.5.3 Axillo-inguinal (AI) Anastomosis
1.5.4 Anterior Interinguinal (AII) Anastomosis
1.5.5 Posterior Interinguinal (PII) Anastomosis
1.6 Lymphatic Drainage and Regional Lymph Node Groups of Different Body Parts
1.6.1 Lymphatic Drainage of the Scalp and Face
1.6.2 Lymphatic Drainage of the Neck
1.6.3 Lymphatic Drainage of the Trunk
1.6.4 Lymphatic Drainage of the Upper Extremity
1.6.5 Lymphatic Drainage of the Lower Extremity
References
Recommended Reading
2 Physiology
2.1 Introduction
2.2 Heart and Circulation
2.3 Blood Pressure
2.3.1 Blood Capillary Pressure
2.4 Capillary Exchange
2.4.1 Diffusion
2.4.2 Osmosis and Osmotic Pressure
2.4.3 Colloid Osmosis and Colloid Osmotic Pressure
2.4.4 Filtration and Reabsorption
2.5 Physiology of the Lymphatic System
2.5.1 Lymph Time Volume and Transport Capacity of the Lymphatic System
2.5.2 Safety Factor of the Lymphatic System
2.6 Insufficiency of the Lymphatic System
2.6.1 Dynamic Insufficiency
2.6.2 Mechanical Insufficiency
2.6.3 Combined Insufficiency
2.7 Edema and Lymphedema at a Glance
2.7.1 Edema
2.7.2 Lymphedema
2.8 Understanding Starling’s Equilibrium
2.8.1 Process 1
2.8.2 Process 2
2.8.3 Process 3
2.8.4 Process 4
2.8.5 Process 5
Recommended Reading
3 Pathology
3.1 Lymphedema
3.1.1 Definition
3.1.2 Incidence and Prevalence of Lymphedema
3.1.3 Lymphedema Incidence among Non–Breast Cancer Patients
3.2 Lymphedema Genetics
3.2.1 Hereditary Lymphedema
3.2.2 Etiology of Lymphedema
3.2.3 Stages of Lymphedema
3.2.4 Grading of Lymphedema Based on Severity
3.2.5 Precipitating Factors for Lymphedema
3.2.6 Avoidance Mechanisms
3.2.7 Complications in Lymphedema
3.3 Axillary Web Syndrome
3.3.1 Definition
3.3.2 Risk Factors
3.3.3 Physiology/Pathophysiology
3.3.4 Incidence, Onset, and Duration of AWS
3.3.5 Assessment and Documentation
3.3.6 Therapeutic Approach
3.4 Impact of Lymphedema on Quality of Life
3.4.1 Personal Views of Lymphedema across the Globe
3.4.2 Impact of Minimal Limb Volume Change on Quality of Life among Survivors with Lymphedema
3.5 Early Identification and Conservative Treatment: Clinical Implications and Interventions
3.5.1 Introduction
3.5.2 Pathophysiology and Presentation of Early Lymphedema
3.5.3 Regional Swelling
3.5.4 Early Identification
3.5.5 Early Intervention
3.5.6 Summary
3.6 Diagnosis of Lymphedema
3.6.1 Diagnosis of Lymphedema—Various Approaches
3.6.2 International Society of Lymphology (ISL) Lymphedema Staging
3.6.3 History
3.6.4 Physical Examination
3.6.5 Medical Education about Lymphedema
3.6.6 Summary
3.7 Evaluation of Lymphedema
3.7.1 Surveillance and Early Intervention
3.8 Research in Lymphedema: Issues of Measurement and Assessment of Occurrence
3.8.1 Measurement Issues in Lymphedema
3.8.2 Issues in Psychosocial Factors Influencing Adaptation to Breast Cancer Lymphedema
3.8.3 Theoretic Framework for Research
3.8.4 Looking to the Future: Imperatives for Research to Support Guidelines for Secondary LE
3.9 Radiation-Induced Brachial Plexopathy and Lymphedema
3.9.1 The Relationship between RIBP and Lymphedema
3.9.2 Therapeutic Approach
3.9.3 Special Considerations to Address with RIBP in the Presence of Lymphedema
3.10 Imaging of the Lymphatic System
3.10.1 Why Image?
3.10.2 Conceptual Basis of Lymphatic Imaging
3.10.3 Lymphoscintigraphy
3.10.4 Lymphography
3.10.5 Ultrasound
3.10.6 Magnetic Resonance Imaging
3.10.7 Combined Multimodal/Fusion Imaging Techniques
3.10.8 Fluorescent Imaging
3.10.9 Summary and the Future
3.11 Therapeutic Approach to Lymphedema
3.11.1 Complete Decongestive Therapy
3.11.2 Massage
3.11.3 Thermo Therapy
3.11.4 Elevation
3.11.5 Sequential Intermittent Pneumatic Compression
3.11.6 Low-Level Laser Therapy
3.11.7 Nutritional Aspects in Lymphedema
3.11.8 Pharmaceutical Options in the Treatment of Lymphedema
3.11.9 Surgical Approaches in the Treatment of Lymphedema
3.12 Chronic Venous and Lymphovenous Insufficiency
3.12.1 Definition of CVI
3.12.2 Postthrombotic Syndrome
3.12.3 Venous Dynamics in the Lower Extremities
3.12.4 Pathophysiology of CVI
3.12.5 Stages of CVI
3.12.6 Complications
3.12.7 Evaluation
3.12.8 Therapeutic Approach
3.13 Wounds and Skin Lesions
3.13.1 Common Skin Changes and Wound Types Associated with Chronic Lymphedema
3.13.2 Wound Bed Preparation
3.13.3 Wound Necrosis
3.13.4 Bacterial Control
3.13.5 Chronic Lymphedema Case Study
3.13.6 Lower Extremity Wound Considerations
3.13.7 A Rationale for MLD in Wound Healing
3.14 Lipedema
3.14.1 Definition of Lipedema
3.14.2 Pathophysiology of Lipedema
3.14.3 Imaging
3.14.4 Stages and Types of Lipedema
3.14.5 Genetics
3.14.6 Comorbid Conditions in Lipedema
3.14.7 Differentiating Conditions of Obesity and Other Edematous Disorders from Lipedema
3.14.8 Comparison of Lipedema to Other SAT Disorders and Fibromyalgia
3.14.9 Standard Treatment of Lipedema
3.14.10 Nonstandard Treatment of Lipedema
3.14.11 Surgical Treatment of Lipedema
3.14.12 Complete Decongestive Therapy for Lipolymphedema
3.15 Pediatric Lymphedema
3.16 Classification: Primary and Secondary Lymphedema
3.16.1 Milroy's Disease
3.16.2 Differentiation
3.16.3 Imaging Studies Reveal Primary Lymphedema
3.16.4 Severity and Extent
3.16.5 Pathologies Contributing to Edema Formation: Adults and Children
3.16.6 Vascular Anomalies Involving Lymphedema in Children
3.16.7 Summary
3.17 Pediatric Syndromes
3.17.1 Amniotic Band Syndrome
3.17.2 Turner's Syndrome and Noonan's Syndrome
3.17.3 Klippel–Trénaunay Syndrome and Parkes Weber Syndrome
3.17.4 Treatments
3.18 Traumatic Edema
3.18.1 Definition
3.18.2 Pathophysiology
3.18.3 Effects of Inflammation on the Lymphatic System
3.18.4 Therapeutic Approach
3.19 Inflammatory Rheumatism
3.19.1 Definition
3.19.2 Anatomy of a Synovial Joint
3.19.3 Pathophysiology
3.19.4 Effects on the Lymphatic System
3.19.5 Therapeutic Approach
3.20 Reflex Sympathetic Dystrophy
3.20.1 Definition
3.20.2 Pathology and Stages
3.20.3 Lymphatic Involvement
3.20.4 Therapeutic Approach
3.20.5 Cyclic Idiopathic Edema
3.20.6 Complete Decongestive Therapy
References
Recommended Reading
4 Complete Decongestive Therapy
4.1 Introduction
4.2 History and Background
4.2.1 Discovery of the Lymphatic System
4.2.2 Development of Complete Decongestive Therapy
4.3 Goal of Complete Decongestive Therapy
4.4 Components of Complete Decongestive Therapy
4.4.1 Manual Lymph Drainage
4.5 Compression Therapy
4.5.1 Effects of Compression Therapy
4.5.2 Laplace's Law
4.5.3 Compression Bandages
4.5.4 Compression Garments
4.6 Exercises and Lymphedema
4.6.1 Breathing Exercises
4.6.2 Resistive Exercises
4.6.3 Aerobic Exercises for Lymphedema
4.7 Skin and Nail Care
4.8 The Two-Phase Approach in Lymphedema Management
4.8.1 Intensive Phase
4.8.2 Self-Management Phase
4.9 Documentation Techniques for Lymphedema
4.10 Complete Decongestive Therapy for Cancer Survivors
4.10.1 Introduction
4.10.2 Surgery
4.10.3 Radiation Therapy
4.10.4 Breast Radiation
4.10.5 Chemotherapy
4.10.6 Targeted Therapy
4.10.7 Guidelines for Safe Complete Decongestive Therapy Intervention
4.10.8 Summary
References
Recommended Reading
5 Treatment
5.1 General Considerations
5.2 Application of Basic MLD Techniques on Different Parts of the Body
5.2.1 Lateral Neck and Submandibular Area
5.2.2 Abbreviated Neck Sequence
5.2.3 Posterior Neck and Occipital Area
5.2.4 Face
5.2.5 Posterior Thorax
5.2.6 Lumbar Area
5.2.7 Anterior Thorax
5.2.8 Abdomen (Superficial and Deep Manipulations)
5.2.9 Upper Extremity
5.2.10 Lower Extremity
5.3 Treatment Sequences
5.3.1 Truncal Lymphedema
5.3.2 Unilateral Secondary Upper Extremity Lymphedema
5.3.3 Bilateral Secondary Upper Extremity Lymphedema
5.3.4 Unilateral Secondary Lower Extremity Lymphedema
5.3.5 Bilateral Secondary Lower Extremity Lymphedema
5.3.6 Unilateral Primary Lower Extremity Lymphedema
5.3.7 Bilateral Primary Lower Extremity Lymphedema
5.3.8 Genital Lymphedema
5.3.9 Phlebolymphostatic Edema
5.3.10 Lipolymphedema
5.4 Head and Neck Lymphedema
5.4.1 Introduction
5.4.2 Etiology
5.4.3 HNL after Cancer Treatment
5.4.4 Evaluation
5.4.5 Treatment of HNL
5.4.6 Compression for HNL
5.4.7 Elastic Therapeutic Tape
5.4.8 Supplemental MLD Sequences
5.4.9 Summary
5.5 Elastic Taping for Lymphedema
5.5.1 General Information and Effectiveness
5.5.2 Safety/Complications
5.5.3 Indications and Contraindications
5.5.4 Preparation and Materials
5.5.5 Application
5.5.6 Patient Education
5.5.7 Removal
5.6 Treatment Strategies for Common Complications of Lymphedema
5.6.1 Surgical Scars
5.6.2 Debulking Scars
5.6.3 Hyperkeratosis
5.6.4 Abnormal Folds
5.6.5 Odors and Odor Control
5.6.6 Fungal Infections
5.6.7 Radiation Trauma
5.6.8 Papillomas
5.6.9 Lymph Cysts and Varicosities
5.6.10 Collateral Veins
5.6.11 Limb Paralysis
5.6.12 Self-Induced Lymphedema (Artificial, Factitious)
5.6.13 Malignant Lymphedema
5.6.14 Cellulitis
5.7 Adapting CDT to the Pediatric Patient
5.7.1 Avoiding High-Risk Treatment
5.7.2 Moderate-Risk Treatments
5.7.3 Complete Decongestive Therapy for the Child
5.7.4 Practical Guidelines for Pediatric Patients
5.7.5 Limitations of CDT
5.7.6 Age-Related Adaptations of CDT: From Birth to First Steps
5.7.7 Age-Related Adaptions of CDT: From Standing Age to Toddler and Older
5.7.8 Special Considerations for Compression Materials
5.7.9 Summary
5.8 CDT Treatment Protocol Variations: Primary and Secondary Lymphedema
5.8.1 Adaptations for the Primary Lymphedema Patient
5.8.2 Adaptations for the Secondary Lymphedema Patient
5.8.3 Underlying Diagnosis and Surgical Treatment Leading to the Development of Lymphedema
5.9 Adapting CDT to the Palliative Patient
5.9.1 Set Realistic Goals
5.9.2 Strengths and Limitations of Each CDT Modality
5.9.3 CDT Management of Generalized Edema
5.9.4 Conclusion
5.10 Lipedema Treatment: Understanding the Diagnosis and Patient Profile
5.10.1 Misguidance and Misdiagnosis
5.10.2 Psychological Perspective and Personality Attributes
5.10.3 Identifying Lipedema and Adapting Treatment
5.10.4 Practical Guidelines for Therapy
5.10.5 Alternative Treatments
5.10.6 Compression Garments
5.11 Application of Compression Bandages
5.11.1 Required Materials
5.11.2 Lymphedema Bandaging: Selecting Foam Padding
5.11.3 Lymphedema Bandaging: Practical Guidelines
5.11.4 Upper Extremity Bandaging
5.11.5 Lower Extremity Bandaging
5.12 Bandaging Procedures Using Foam Padding
5.12.1 Arm Bandaging Procedure Using Foam Padding (in Detail)
5.12.2 Leg Bandaging Procedure Using Foam Padding (in Detail)
5.13 Genital Lymphedema Treatment
5.13.1 Secondary Genital Lymphedema
5.13.2 Primary Genital Lymphedema
5.13.3 Predisposition to Develop Lymphedema
5.13.4 Complications
5.13.5 Surgical Treatment
5.13.6 Conservative Therapy
5.14 Truncal Lymphedema
5.14.1 Lymphedema of the Thorax
5.14.2 Lymphedema of the Abdomen
5.15 Bandaging in the Presence of Wounds
5.15.1 Precautions and Contraindications
5.15.2 Treat the Wound
5.15.3 Apply Compression
5.15.4 Negative Pressure Wound Therapy and Compression
5.15.5 Summary
5.16 Measurements for Compression Garments
5.16.1 Measuring for Stockings and Pantyhose
5.16.2 Measuring for Arm Sleeves
5.16.3 Measuring for Hand and Finger Compression Garments
5.16.4 Compression Neck and Chin Straps and Face Masks
5.16.5 Compression Garments for the Upper Thorax and Breast
5.16.6 Fitting Compression Garments upon Delivery
5.17 Compression Bandaging Alternatives: Guidelines to Choosing the Right Home Care Systems
5.17.1 Rationale for an Alternative
5.17.2 Important Considerations
5.17.3 Product Categories
5.17.4 Maximizing the Benefits of Alternative Devices
5.17.5 Patient Education and Long-Term Compression Therapy
5.17.6 Suggested Modifications by Product Category
5.18 Treatment Considerations in Managing the Morbidly Obese Patient
5.18.1 The Problem
5.18.2 Equipment
5.18.3 Treatment Challenges
5.19 Lymphedema Therapy in the Home
5.19.1 Complications in the Home Care Setting
5.19.2 The Home Environment—Opportunities and Challenges
5.19.3 A New Care Setting—Administrative Guidelines and Considerations
5.19.4 Appropriate Referral Protocols
5.19.5 The Five Components of CDT in the Home Care Setting
5.19.6 Practical Applications and Useful Tips
5.19.7 Conclusion: Building a Bridge
5.20 Patient Education
5.20.1 Lymphedema Therapists
5.20.2 Self-Bandaging
5.20.3 Exercises
5.20.4 Self-MLD
5.20.5 Precautions
5.20.6 Traveling with Lymphedema
5.20.7 Lymphedema and Air Travel
5.21 Surgical Treatment
5.21.1 Surgical Treatment of Lymphedema
5.21.2 Lymphedema Surgery as Part of an Integrated Lymphedema Treatment System
5.21.3 Breast and Axillary Reconstruction Primer for the Certified Lymphedema Therapist
References
Recommended Reading
6 Administration
6.1 Introduction
6.2 Setting Up a Lymphedema Clinic
6.2.1 Personnel
6.2.2 Required Space
6.2.3 Equipment
6.2.4 Marketing Issues
6.3 Suggested Materials to Start Up a Lymphedema Program
6.4 Reimbursements and Billing
6.4.1 Current Procedural Terminology Codes
6.4.2 ICD-10 Codes
6.5 Sample Forms and Templates
Recommended Reading
Index
| An aparitie | 2017 |
| Autor | Joachim Ernst Zuther , Steve Norton |
| Dimensiuni | 18.3 x 3 x 25.9 cm |
| Editura | Thieme |
| Format | Hardback |
| ISBN | 9781626234338 |
| Limba | Engleza |
| Nr pag | 600 |

Clientii ebookshop.ro nu au adaugat inca opinii pentru acest produs. Fii primul care adauga o parere, folosind formularul de mai jos.