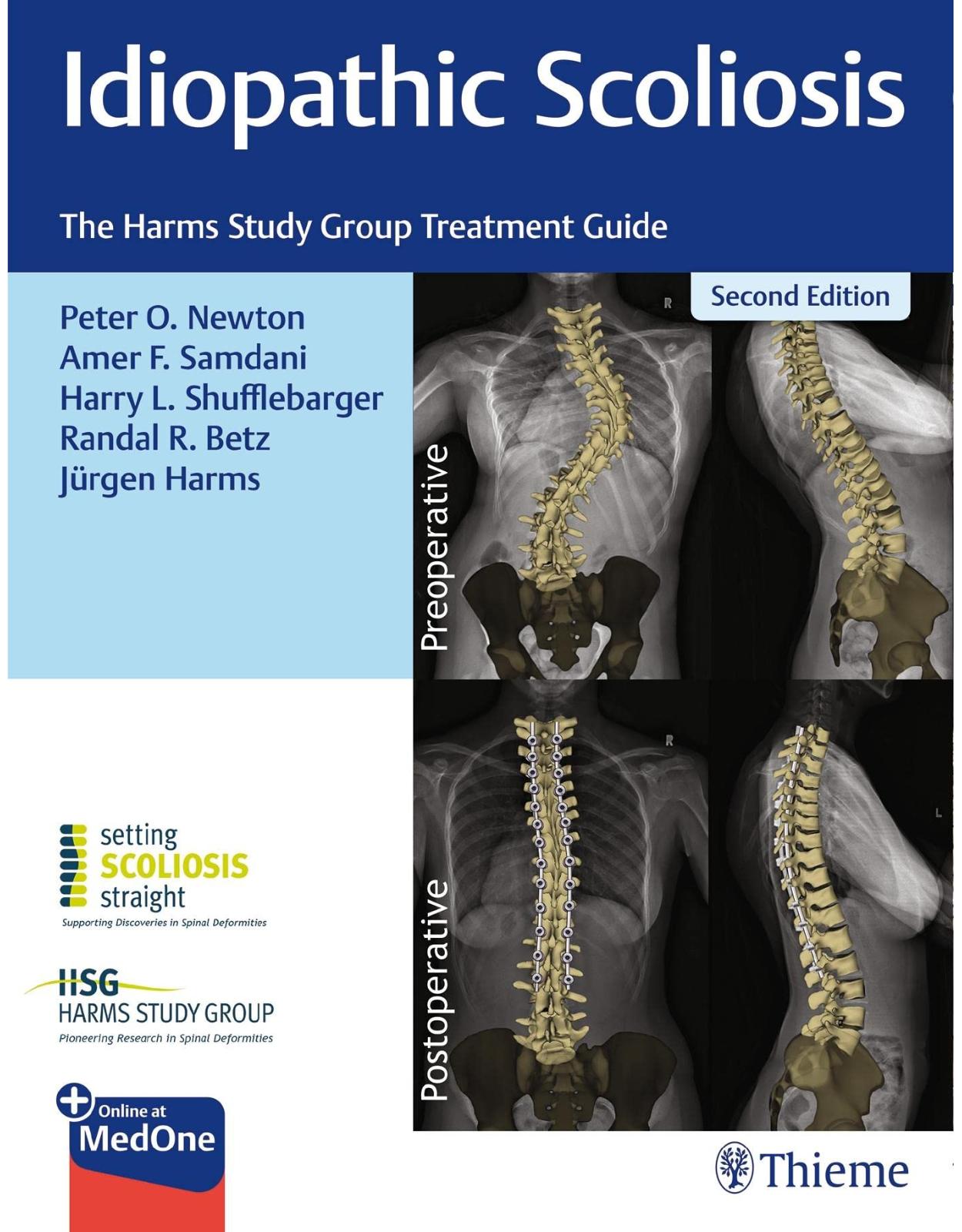
Idiopathic Scoliosis
Livrare gratis la comenzi peste 500 RON. Pentru celelalte comenzi livrarea este 20 RON.
Disponibilitate: La comanda in aproximativ 4-6 saptamani
Editura: Thieme
Limba: Engleza
Nr. pagini: 364
Coperta: Hardcover
Dimensiuni: 22.86 x 2.54 x 29.21 cm
An aparitie: 17 Nov. 2021
Description:
The definitive practical reference on managing idiopathic scoliosis from world-renowned experts
Idiopathic Scoliosis: The Harms Study Group Treatment Guide, Second Edition, edited by Peter O. Newton, Amer F. Samdani, Harry L. Shufflebarger, Randal R. Betz, and Jürgen Harms and written by an impressive group of experts reflects treatment advances made in the last decade. Greater understanding of the etiology and improved 3D anatomy has resulted in significant strides in clinical management of scoliosis. This richly illustrated book presents all facets of evaluation and treatment of abnormal curvature of the spine, supported by a solid foundation of evidence-based data culled from the prestigious Harms Study Group.
Divided into four sections and 31 chapters, this one-stop reference encompasses the full spectrum of surgical and nonoperative interventions—from early treatments to modern novel growth modulation techniques. In this second edition, each chapter has been updated and several new ones have been added, reflecting current literature, practice, and expert perspective. Throughout the book, masters share clinical pearls and firsthand knowledge on managing diverse types of adolescent idiopathic spinal deformity, with the common goal of improved patient outcomes.
Key Highlights
Innovative topics include teamwork and safety in spine surgery, halo traction for large curves, anterior growth modulation, intraoperative neuromonitoring, and kyphosis restoration in scoliosis surgery
Surgical chapters follow a consistent layout, encompassing rationales, techniques, and outcomes
Postoperative chapters feature discussion of long-term clinical and radiographic outcomes, infections, complications, and rapid post-op recovery
A wealth of illustrations enhance the reader's knowledge of specific techniques
This comprehensive textbook is essential reading for orthopaedic and neurosurgical residents, fellows, and researchers. Young spine surgeons embarking on their careers and senior surgeons who wish to remain up-to-date on new techniques for treating adolescent idiopathic scoliosis will also benefit from this illuminating resource.
Table of Contents:
Section I Evaluation and Management
1 History of Scoliosis Treatment
1.1 Introduction
1.2 Lewis Sayre, the Father of Orthopaedics
1.3 Operative Treatment
1.4 Russell A. Hibbs and Frederick H. Albee
1.5 John Robert Cobb and the Cobb Angle for Scoliosis
1.6 Fusion, Casting, and Prolonged Bedrest
1.7 Paul R. Harrington
1.8 Allen F. Dwyer and Anterior Instrumentation
1.9 Zielke Instrumentation Anterior Surgery..
1.10 Kostuik–Harrington Anterior Instrumentation Utilizing Harrington Screws
1.11 Luque Segmental Fixation
1.12 Cotrel–Dubousset Instrumentation and 3D Concepts of AIS
1.13 History of Pedicle Screws and Plates: King, Boucher, Roy-Camille
1.14 Polyaxial Screws in Spine Surgery
1.15 Segmental Application of Polyaxial Screw Constructs
1.16 Suk and Harms Thoracic Screws in Deformity
1.17 Spinal Instrumentation: Rods
1.18 Scoliosis Classification Systems
1.19 Osteotomies for Kyphosis and Scoliosis.
1.19.1 Thoracoplasty for Rib Prominence
1.20 3D Understanding of Scoliosis and the Future
1.21 History of Collaborative Research in Scoliosis
1.22 Tips/Pearls
2 Etiological Theories of Idiopathic Scoliosis
2.1 Introduction
2.2 Biomechanics of the Upright Human Spine as Related to the Sagittal Profile, Dorsal Shear Loads
2.2.1 Evolution of the Human Pelvis, Pelvic Lordosis
2.2.2 Dorsal Shear Loads Acting on the Human Spine
2.2.3 Di?erences in Sagittal Spinal Alignment
2.2.4 Preexistent Rotation of the Nonscoliotic Spine
2.3 Animal Models.
2.3.1 Quadrupedal Animal Models
2.3.2 Bipedal Animal Models
2.3.3 Genetic Animal Models
2.3.4 Human Model
2.4 The Role of the Intervertebral Disc
2.5 Current Understanding of Genetics in AIS
2.5.1 Genome-Wide Association Studies
2.5.2 Di?erential Roles of Genetics and Environment Factors in Initiation/Progression of Deformity
2.5.3 Clinical Implications
2.5.4 Future Trends of Genetic Studies.
2.6 Bone Growth and Metabolism in Adolescent Idiopathic Scoliosis
2.6.1 Abnormal Skeletal Growth
2.6.2 Body Composition and Metabolic Dysfunction
2.6.3 Low Bone Mineral Density, Abnormal Bone Structure and Qualities
2.6.4 Abnormal Bone Turnover and Bone Cells Activity
2.6.5 Lifestyle Factors Associated with Low BMD and Poor Bone Quality
2.6.6 Bone Mass and Bone Qualities as Prognostic Factors of Curve Progression?
2.6.7 Potential Clinical Intervention and Lifestyle Modification Targeting Bone Health that Might A?ect the Curve Progression in Early AIS
2.7 Central Nervous System
2.7.1 Neurophysiological Dysfunction
2.7.2 Neuromorphological Changes (MRI-Based Studies).
2.8 Discussion
2.9 Tips/Pearls
3 Prevalence and Natural History
3.1 Introduction
3.2 School Screening
3.2.1 Prevalence According to Genetic Factors.
3.2.2 Prevalence by Age
3.2.3 Prevalence by Gender
3.2.4 Prevalence by Curves
3.3 Natural History
3.4 Curve Progression
3.4.1 Curve Characteristics
3.4.2 Stage of Skeletal Growth
3.5 Back Pain
3.6 Cardiopulmonary Function
3.7 Psychosocial Issues and Cosmesis
3.8 Future Insights into the Natural History of Scoliosis.
3.9 Tips/Pearls
4 Clinical and Radiographic Evaluation of Patients with Scoliosis
4.1 Introduction
4.2 History and Clinical Presentation
4.3 Physical Examination
4.4 Radiographic Evaluation
4.5 Assessment of Skeletal Maturity
4.6 Conclusion
4.7 Tips/Pearls
5 Nonoperative Management of Adolescent Idiopathic Scoliosis.
5.1 Introduction
5.2 Screening
5.3 History of Bracing
5.4 Types of Braces
5.5 Evidence for Bracing
5.6 BrAIST and Factors Impacting Brace Success
5.6.1 Factors Impacting Brace E?ectiveness
5.6.2 Psychosocial E?ects of Bracing.
5.7 The Authors’ Recommended Treatment Method
5.8 Bracing
5.9 Conclusion and Future Directions
5.10 Tips/Pearls
6 Classification of Adolescent Idiopathic Scoliosis for Surgical Intervention
6.1 Introduction
6.2 Classification
6.2.1 Historical Perspective
6.2.2 King Classification
6.2.3 Lenke Classification
6.2.4 SRS Three-Dimensional Classification System.
6.3 Conclusion
6.4 Tips/Pearls
7 Biomechanics and Correction of Scoliosis
7.1 Introduction: Three-Dimensional Morphology of Scoliosis and Spine Biomechanics
7.2 Deformity Correction Mechanics
7.3 Growth Modulation Instrumentation Mechanics
7.4 Multisegmental Correction Mechanics and Failure Modes
7.5 Bone Implant Interface Failure Mode (Pullout and Nonaxial Loads)
7.6 Long-Term Failure (Cyclic Loading)
7.7 Complex Deformity Correction Problems (Proximal Junctional Kyphosis and Proximal Junctional Failure)
7.8 Conclusion
7.9 Tips/Pearls
8 Benefits of Teams and Teamwork in Spine Surgery Quality, Safety, and Value
8.1 Introduction
8.2 Communication
8.3 Building Safety and Belonging
8.4 Team of Teams: Creating Shared Consciousness and Purpose
8.5 A Tale of Two Team Building E?orts: Children’s Hospital of Philadelphia and Children’s Hospital of New York
8.5.1 The CHOP Experience: The Value of Dedicated Surgical Teams: Bringing NASA and NASCAR Wisdom to Your Spine Operating Room
8.5.2 Improving Throughput at Children’s Hospital of New York: Leveraging a Comprehensive Unit-Based Safety Program
8.6 Tips/Pearls
9 Clinical Implications of Three-Dimensional Analysis
9.1 Introduction
9.2 History of Radiographic Analysis
9.3 Three-Dimensional Reference Plane Definitions
9.3.1 Coronal Plane
9.3.2 Sagittal Plane
9.3.3 Transverse or Axial Plane.
9.3.4 Plane of Maximum Curvature
9.3.5 The Role of MRI and CT Imaging in AIS
9.3.6 Synchronized Biplanar Radiographic 3D Reconstruction
9.4 2D Radiograph to 3D Measurement Conversion Techniques
9.5 Conclusion
9.6 Tips/Pearls
Section II Surgical Considerations
10 Selective versus Nonselective Fusion for Adolescent Idiopathic Scoliosis
10.1 Introduction
10.2 Indications and Criteria
10.3 Technical Aspects for Successful Selective Fusion.
10.3.1 Selection of Fusion Levels
10.4 Correction Mechanics and Desired Correction
10.4.1 Selective Thoracic Fusion.
10.5 Outcomes Following Selective Fusion
10.6 Complications
10.7 Conclusion
10.8 Tips/Pearls
11 Selection of Fusion Levels
11.1 Background/Historic Context 114 11.2 History and Physical Examination
11.3 Radiographic Evaluation
11.4 Operative Algorithm/Goals
11.5 Anterior Spinal Fusion Level Selection
11.6 Posterior Spinal Fusion Level Selection
11.7 UIV Selection in Posterior Fusions
11.7.1 Upper Thoracic and Main Thoracic UIV
11.7.2 Thoracolumbar Upper Instrumented Vertebra
11.8 LIV Selection in Posterior Fusions
11.8.1 Main Thoracic Lower Instrumented Vertebra
11.8.2 Thoracolumbar Lower Instrumented Vertebra
11.9 Detailed Discussion of Lenke Curve Types
11.9.1 Type 1: Main Thoracic Curves.
11.9.2 Type 2: Double Thoracic Curves.
11.9.3 Type 3: Double Major Curves
11.9.4 Type 4: Triple Major Curves
11.9.5 Type 5: Thoracolumbar/Lumbar Curves
11.9.6 Type 6: Thoracolumbar/Lumbar Main Thoracic Curves
11.10 Other Considerations
11.11 Conclusion
11.12 Tips/Pearls
12 Posterior Correction Techniques in Adolescent Idiopathic Scoliosis.
12.1 Introduction
12.2 Implant Properties.
12.3 Other Rod Materials
12.4 Correction Maneuvers
12.4.1 Compression–Distraction
12.4.2 Rod Derotation Maneuver
12.4.3 In Situ Contouring
12.4.4 Coronal and Sagittal Translation
12.4.5 En Bloc Vertebral Derotation
12.4.6 Segmental Vertebral Derotation
12.4.7 Derotation via Di?erential Rod Contouring
12.4.8 Cantilever Technique
12.4.9 Traction
12.5 The Authors’ Preferred Technique of Correction in Adolescent Idiopathic Scoliosis
12.6 En Bloc Spinal Derotation Technique
12.7 Segmental Spinal Derotation
12.8 The Authors’ Preferred Technique for Reducing Spinal Deformity
12.9 Conclusion
12.10 Tips/Pearls
13 Halo Traction in Large Idiopathic Scoliotic Curves Walter Klyce and Paul D. Sponseller
13.1 Introduction
13.2 Traction: The Risks and Benefits
13.3 Preferred Methods of Preoperative Traction
13.3.1 Halo-Femoral Traction
13.3.2 Halo-Gravity Traction
13.4 Complications and Contraindications.
13.5 Tips/Pearls
14 Indications and Techniques for Anterior Release and Fusion
14.1 Introduction
14.2 History and Evolution of Anterior Approaches
14.3 Complications
14.4 Pulmonary Function
14.5 Modern Approach
14.6 Crankshaft
14.7 Lack of Posterior Elements/Neuromuscular Scoliosis.
14.8 Techniques
14.9 Thoracotomy
14.10 Thoracoscopy
14.11 Thoracoabdominal Approach
14.12 Conclusion
14.13 Tips/Pearls
15 Posterior Releases: Pontes and Three-Column Osteotomies.
15.1 Introduction
15.2 Classification and History.
15.2.1 Classification of Posterior-Based Osteotomies
15.2.2 History of Posterior Column Osteotomies (Schwab Type 2/Ponte/Smith-Petersen)
15.2.3 Pedicle Subtraction Osteotomies (Type 3/4)
15.2.4 Vertebral Column Resections (Type 5/6)
15.3 Surgical Techniques
15.3.1 Posterior Column Osteotomies/Schwab Type 2
15.4 Complications
15.4.1 Posterior Column Osteotomy/Schwab Type 2
15.4.2 Three-Column Osteotomy/Schwab Types 3, 4, 5, and 6
15.5 Conclusion
15.6 Tips/Pearls
16 Surgical Treatment of the Right Thoracic Curve Pattern
16.1 Introduction
16.2 Deformity Classification
16.2.1 Three-Dimensional Analysis of the MT Curve
16.3 Decisions Relating to Surgical Treatment
16.3.1 Is a Surgically Instrumented Fusion Indicated?
16.3.2 The Inclusion of Minor Curves in the Fusion.
16.3.3 To What Extent Should the Thoracic Curve Be Corrected for Ideal Balance?
16.3.4 What Levels Should Be Included in the Fusion?
16.3.5 What Is the Best Approach?
16.3.6 When Is an Anterior Release Indicated?
16.4 Surgical Techniques
16.4.1 Posterior Spinal Instrumentation and Fusion.
16.4.2 Open Anterior Spinal Instrumentation and Fusion
16.4.3 Thoracoscopic Anterior Spinal Instrumentation and Fusion
16.5 Summary of Treatment
16.5.1 Recommendations for Lenke Type 1AR Curves
16.5.2 Lenke Type 1AL/1B Curves
16.5.3 Lenke Type 1C Curves
16.6 Conclusion 184 16.7 Tips/Pearls
17 Assessment and Management of Shoulder Balance
17.1 Introduction
17.2 History and Relevance of Shoulder Balance
17.2.1 Shoulder Balance in Normal Adolescents
17.2.2 Relationship of Shoulder Balance with Outcome Scores
17.3 Assessment of Shoulder Balance
17.3.1 Clinical Evaluation of Shoulder Balance.
17.3.2 Radiographic Evaluation of Shoulder Balance
17.3.3 Authors’ Recommendation
17.3.4 Relationship of Clinical and Radiographic Shoulder Balance
17.4 Curve Patterns/Factors Associated with Shoulder Imbalance
17.4.1 Magnitude and Flexibility of the Proximal Thoracic Curve
17.4.2 Preoperative Shoulder Imbalance
17.4.3 Authors’ Recommendation
17.5 Strategies to Achieve/Correct Shoulder Balance
17.5.1 Upper Instrumented Vertebra Selection
17.5.2 Technique for Deformity Correction and Impact on Shoulder Balance
17.5.3 Relationship of Proximal Thoracic to Main Thoracic Correction
17.5.4 Intraoperative Shoulder Balance Assessment
17.5.5 Authors’ Recommendation
17.6 Postoperative Shoulder Balance
17.6.1 Postoperative Changes in Alignment
17.6.2 Patient-Reported Outcomes with Shoulder Imbalance
17.7 Conclusion
17.8 Tips/Pearls
18 Surgical Treatment of Lumbar and Thoracolumbar Curve Patterns (Lenke V).
18.1 Introduction
18.2 Level Selection and Surgical Technique
18.2.1 Upper and Lower Instrumented Vertebrae
18.2.2 When Does Lenke 5 Become 6?
18.2.3 Ponte Osteotomy in Lenke 5 Curves
18.2.4 Correction Techniques in Lenke 5 Curves
18.2.5 Outcomes in Lenke 5 Curves.
18.3 Discussion
18.4 Tips/Pearls
19 The Surgical Treatment of Double and Triple Curves (Lenke Types 3, 4, and 6)
19.1 Introduction
19.2 Curve Definitions
19.3 Treatment Principles.
19.4 Recent Trends in the Surgical Decision- Making Process
19.5 Surgical Approaches
19.6 Conclusion
19.7 Tips/Pearls
20 Thoracoplasty
20.1 Introduction
20.2 Indications
20.3 Operative Technique.
20.4 Complications
20.5 Postoperative Management
20.6 The Authors’ Institutional Experience with Thoracoplasty
20.7 Conclusion
20.8 Tips/Pearls
21 Kyphosis Restoration in Adolescent Idiopathic Scoliosis
21.1 Introduction
21.2 Background
21.3 Importance of Sagittal Plane Correction
21.4 Surgical Restoration of Kyphosis
21.4.1 General
21.4.2 Curve Attributes.
21.4.3 Release of Spine: Posterior
21.4.4 Anterior Surgery/Video-Assisted Thoracoscopic Surgery
21.5 Posterior-Based Surgery
21.5.1 Type of Fixation
21.5.2 Implant Density
21.5.3 Rod Properties and Techniques
21.6 Conclusion
21.7 Tips/Pearls
Section III Postoperative Management
22 Long-Term Clinical and Radiographic Outcomes of Scoliosis
22.1 Introduction
22.2 Long-Term Clinical Questions Answered
22.2.1 Maintenance of Radiographic Correction
22.2.2 Cosmesis.
22.2.3 Pulmonary Function
22.2.4 Spine Function, Mobility, and Health
22.2.5 Health-Related Quality of Life
22.2.6 Pregnancy and Childbirth
22.2.7 Reoperations at Long-Term Follow-Up
22.2.8 Comparison to Natural History
22.3 Long-Term Clinical Questions Remaining
22.4 Future Directions
22.5 Conclusion
22.6 Tips/Pearls
23 Infection in Adolescent Idiopathic Scoliosis
23.1 Introduction
23.2 Background
23.3 Surveillance Periods for Surgical Site Infection
23.3.1 Early versus Late Surgical Site Infection
23.3.2 Deep versus Superficial Surgical Site Infection
23.4 Early Infections
23.4.1 Background and Incidence
23.4.2 Risk Factors and Prevention
23.4.3 Clinical Presentation and Evaluation
23.4.4 Treatment
23.5 Late Infections
23.5.1 Clinical Features
23.5.2 Evaluation and Initial Management
23.5.3 Surgical Management
23.5.4 Aftercare.
23.6 Conclusion
23.7 Tips/Pearls
24 Complications and Reoperations in Adolescent Idiopathic Scoliosis
24.1 Introduction
24.2 Intraoperative Complications
24.3 Early Postoperative Complications
24.4 Late Postoperative Complications
24.5 Best Practice Guidelines
24.6 Conclusion
24.7 Tips/Pearls
25 Accelerated Pathways
25.1 Introduction
25.2 Background
25.3 Preoperative Considerations
25.3.1 Nutrition
25.3.2 Pulmonary
25.3.3 Gastrointestinal
25.3.4 Patient/Parent Expectations
25.4 Postoperative Management
25.4.1 Overview
25.4.2 Pain Management
25.4.3 Nutrition and Bowel Management
25.4.4 Mobilization
25.4.5 Care Pathways.
25.5 Conclusion
25.6 Tips/Pearls
26 Untreated Late-Onset Idiopathic Scoliosis and Revision Surgery in Adults
26.1 Introduction
26.2 Untreated Adolescent Idiopathic Scoliosis
26.3 Preoperative Assessment and Nonoperative Treatment
26.4 Complications an
26.5 Proximal and Distal Junctional Kyphosis
26.6 Revision Surgery, Alignment, and HRQOL
26.7 Flatback
26.8 Long-Term Follow-up after Adolescent Fusion
26.9 Tips/Pearls
Section IV Miscellaneous Topics
27 Osteobiologic Agents for Spinal Fusion Benjamin D. Roye and Stephen G. George
27.1 Introduction
27.2 The Biology of Spinal Fusion
27.3 Osteobiologic Products and Spinal Fusion
27.3.1 Autogenous Bone Graft
27.3.2 Allogenic Bone Graft
27.3.3 Cadaveric Allograft
27.3.4 Ceramics.
27.3.5 Demineralized Bone Matrix
27.3.6 Osteoinductive Proteins
27.3.7 Platelet Concentrates
27.3.8 Growth and Di?erentiation Factor-5
27.4 Conclusion
27.5 Tips/Pearls
28 Intraoperative Neuromonitoring
28.1 Introduction
28.2 History.
28.2.1 Stagnara Wake-up Test
28.2.2 Ankle Clonus Test
28.3 Neuromonitoring
28.3.1 Somatosensory Evoked Potentials.
28.3.2 Transcranial Motor Evoked Potentials
28.3.3 Multimodality.
28.3.4 Triggered Electromyography
28.3.5 Descending Neurogenic Evoked Potentials
28.3.6 H-Reflex
28.3.7 D-Wave Monitoring
28.4 Anesthesia and Other Agents
28.4.1 Inhalational Agents
28.4.2 Total Intravenous Anesthesia
28.5 Other Considerations
28.5.1 Steroids.
28.6 Change in Intraoperative Neuromonitoring
28.6.1 Significant Change
28.6.2 Team Response to Intraoperative Neuromonitoring Alert
28.6.3 Timing of Change and Time to Return
28.6.4 Rate of Injury in Adolescent Idiopathic Scoliosis
28.6.5 Risk Factors for Changes in Intraoperative Neuromonitoring
28.6.6 Delayed Postoperative Neurologic Deficit
28.7 Case Examples
28.7.1 Case Example 1.
28.7.2 Case Example 2.
28.7.3 Case Example 3.
28.7.4 Case Example 4.
28.7.5 Case Example 5.
28.8 Conclusion
28.9 Tips/Pearls
29 Anterior Growth Modulation
29.1 Introduction
29.2 Clinical Application and Potential
29.3 Surgical Technique
29.4 Reported Outcomes
29.5 Conclusion
29.6 Tips/Pearls
30 Managing the Preadolescent Curve: Early Fusion versus Posterior Distraction
30.1 Introduction
30.2 Spinal and Thoracic Growth
30.3 Surgical Alternatives.
30.4 Growth-Friendly Techniques.
30.5 Instrumented Fusion.
30.6 Conclusion
30.7 Tips/Pearls
31 The Development and Evolution of the Harms Study Group Registry.
31.1 Introduction
31.2 Development of a Study Group
31.3 Database Evolution
31.4 Research Study Development and Evolution
31.5 Surgeon/Site Participation.
31.5.1 Data Quality Assurance
31.5.2 Study Group Strategic Plan: Formation of a 501(c)(3) Nonprofit
31.6 The Power of Large Registries: Beyond the Research
31.7 Conclusion
31.8 Tips/Pearls
Index
| An aparitie | 17 Nov. 2021 |
| Autor | Peter Newton, Amer Samdani, Harry Shufflebarger, Randal Betz, Jürgen Harms |
| Dimensiuni | 22.86 x 2.54 x 29.21 cm |
| Editura | Thieme |
| Format | Hardcover |
| ISBN | 9781684200559 |
| Limba | Engleza |
| Nr pag | 364 |
| Versiune digitala | DA |
-
81100 lei 72900 lei


Clientii ebookshop.ro nu au adaugat inca opinii pentru acest produs. Fii primul care adauga o parere, folosind formularul de mai jos.