Gynaecology for the Obstetrician
Livrare gratis la comenzi peste 500 RON. Pentru celelalte comenzi livrarea este 20 RON.
Disponibilitate: La comanda in aproximativ 4 saptamani
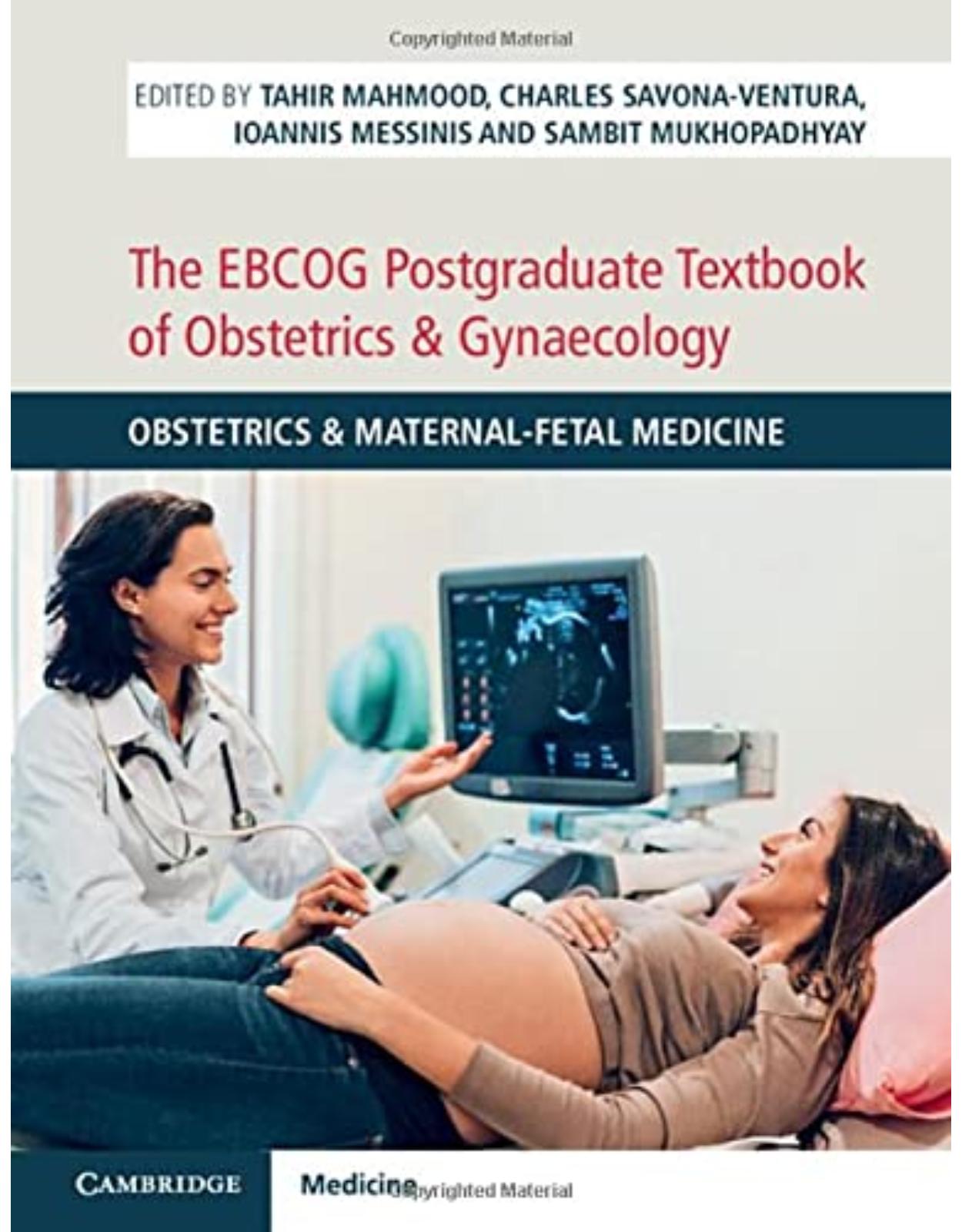
Autor: Swati Jha, Priya Madhuvrata
Editura: Cambridge University Press
Limba: Engleza
Nr. pagini: 180
Coperta: Paperback
Dimensiuni: 157 x 234 x 9 mm
An aparitie: 31 July 2023
Description:
In this era of specialisation, obstetricians are becoming increasingly skilled at their jobs and deskilled in areas outside their expertise. In recent years, the education and training curricula for obstetrics and gynaecology has changed, with obstetricians expected to manage women with complex gynaecological problems encountered during pregnancy and the postnatal period competently, despite training and curricula not covering these problems in detail. Exploring common gynaecological problems such as ovarian cysts, management of vaginal prolapse and female genital mutilation, this practical book offers guidance for managing these conditions throughout the different stages of pregnancy and post-partum. Each chapter has a section on good governance, discussing salient points for clinical practice to improve patient safety and satisfaction, as well as reducing complaints and litigation. This hands-on book provides obstetricians around the globe with the evidence-based knowledge needed to deliver high quality care to pregnant women.
Table of Contents:
Chapter 1 Ovarian Cysts in Pregnancy
1.1 Introduction
1.2 Types of Cysts
1.3 Clinical Presentation and Complications
1.3.1 Torsion
1.3.2 Ovarian Cyst Rupture and Haemorrhage
1.3.3 Mass Effect: Obstruction of Labour
1.4 Diagnostic Evaluation
1.4.1 Imaging
1.4.2 Tumour Markers
1.5 Management
1.5.1 Expectant Management
1.5.2 Ultrasound-Guided Fine Needle Aspiration
1.5.3 Surgical Management
1.5.3.1 Elective versus Emergency Surgery
1.5.3.2 Cystectomy versus Oophorectomy
1.5.3.3 When to Operate?
1.5.3.4 Obstetrical Considerations and Fetal Monitoring
1.6 Post-Natal Follow-Up
1.7 Conclusion
References
Chapter 2 Fibroids in Pregnancy
2.1 Introduction
2.2 Types of Fibroids
2.3 The Effect of Pregnancy on Fibroids
2.4 The Effect of Fibroids on the Pregnancy
2.4.1 Multiple Large Fibroids in the Anterior Wall and Lower Segment
2.4.1.1 Maternal Complications
2.4.1.2 Fetal Complications
2.4.2 Large Cervical Fibroids
2.4.2.1 Cervical Fibroid Polyps in the Vagina
2.5 Antenatal Management of Women with Fibroids
2.6 Counselling about the Risks and Impact of Fibroids on Mode of Delivery
2.6.1 Vaginal Delivery
2.6.2 Caesarean Section
2.7 Delivery with History of Previous Myomectomy
2.8 Post-Natal Management of Women with Fibroids
References
Chapter 3 Cervical Abnormalities in Pregnancy
3.1 Introduction
3.1.1 LLETZ and Obstetric Outcomes
3.1.2 Loop Depth and the Risk of Preterm Labour
3.1.3 Cervical Length Screening
3.2 Abnormal Smears
3.2.1 Introduction
3.2.2 Abnormal Smears and Colposcopy during Pregnancy
3.3 Cervical Cancer in Pregnancy
3.3.1 Introduction
3.3.2 Staging of Cancer
3.3.3 Treatment
3.4 Benign Cervical Lesions in Pregnancy
References
Chapter 4 Vulval Disorders in Pregnancy
4.1 Assessment of the Patient
4.1.1 History Taking
4.1.2 Vulval Examination
4.1.3 Investigations
4.1.3.1 Diagnostic Vulval Biopsy
4.1.3.2 Vaginal and Vulval Swabs
4.1.3.3 The Vulval Clinic
4.1.4 Specific Vulval Skin Diseases
4.2 Management of Vulval Skin Conditions
4.2.1 General Principles
4.2.2 Correct Barrier Function
4.2.3 Using Topical Steroids on the Vulva
4.3 Lichen Sclerosus
4.4 Contact Dermatitis
4.5 Candidiasis
4.6 Bartholin Gland Cysts
4.7 Vulvodynia
4.8 Conclusions
Further Resources
References
Chapter 5 Congenital Uterine Malformations and Vaginal Anomalies
5.1 Introduction
5.1.1 Classification of Congenital Female Genital Tract Malformations
5.2 Septate Uterus
5.3 Bicornuate, Didelphys and Unicornuate Uteri
5.4 Vaginal Septum and Repair
5.5 Counselling and Reproductive Outcomes
5.6 Conclusion
References
Chapter 6 Vaginal Prolapse and Previous Prolapse Surgery
6.1 Introduction
6.2 Antenatal
6.2.1 Women with Pre-existing Prolapse or First Presentation in Pregnancy
6.2.2 Women with Previous Prolapse Surgery
6.3 Intrapartum
6.3.1 Women with Pre-existing Prolapse or First Presentation in Pregnancy
6.3.2 Women with Previous Prolapse Surgery
6.4 Post-Partum
6.5 Clinical Dilemmas
6.6 Conclusion
References
Chapter 7 Urinary Tract Problems in Pregnancy
7.1 Urinary Incontinence
7.1.1 Previous Surgery for Stress Urinary Incontinence
7.2 Urinary Retention during Pregnancy and Post-Partum (URPP)
7.2.1 Pathophysiology
7.2.2 Assessment and Management of URPP: Antenatal, Perinatal and Post-Partum
7.2.3 Antenatal Urinary Retention
7.2.4 Peripartum Urinary Retention
7.2.5 Post-Partum Urinary Retention (PPUR)
7.3 Urinary Diversions and Mitrofanoffs during Pregnancy
7.4 Renal Transplant
7.4.1 Effects of Transplant on Pregnancy
7.4.2 Labour and Delivery
7.4.3 Immunosuppressive Agents During the Perinatal Period
7.5 Congenital Anomalies of the Urinary Tract
7.5.1 Exstrophy-Epispadias Complex
7.5.2 Persistent Cloaca
7.5.3 Spinal Dysraphism
7.5.4 Congenital Vesicoureteric Reflux (CVUR)
7.6 Conclusion
References
Chapter 8 Previous Third and Fourth Degree Tears
8.1 Background
8.1.1 Antenatal
8.1.2 Intrapartum
8.1.3 Post-Partum
8.2 Clinical Dilemmas
8.3 Conclusion
References
Chapter 9 Management of Post-Partum Retained Placental Remnants
9.1 Introduction
9.2 Diagnosis
9.2.1 Ultrasonography
9.2.2 Other Diagnostic Investigations
9.3 Causative Factors
9.4 Treatment of Post-Partum Placental Remnants
9.4.1 Expectant Management
9.4.2 Medical Management
9.4.3 Surgical Intervention
9.4.3.1 Hysteroscopic Techniques
9.4.3.2 Timing of Surgical Intervention
9.4.3.3 Effectiveness (complete removal rate)
9.4.3.4 Short-Term Complications
9.4.3.5 Longer-Term Outcomes
9.5 Counselling
9.6 Summary
References
Chapter 10 Gestational Trophoblastic Disease (GTD)
10.1 Background
10.2 Antenatal
10.2.1 Prior History of GTD or GTN
10.2.2 Early Pregnancy in GTD or GTN
10.2.2.1 Termination of pregnancy
10.2.2.2 Miscarriage
10.2.2.3 Fetal anomalies and stillbirth
10.2.2.4 Live birth rates
10.2.2.5 Relapse
10.2.2.6 Risk of second molar pregnancy
10.2.3 Twin Pregnancy with a Hydatidiform Mole and Viable Coexistent Fetus
10.2.3.1 Misdiagnosis
10.2.3.2 Complications
10.2.3.3 Termination of Pregnancy
10.2.3.4 Live Birth Rates
10.2.3.5 Risk of Developing GTN
10.3 Intrapartum
10.3.1 Prior History of GTD/GTN and Early Pregnant GTD Patients
10.3.2 Early Pregnant GTN Patients
10.3.3 Twin Pregnancy with a Hydatidiform Mole and Viable Coexistent Fetus
10.4 Post-Partum
10.4.1 Prior History of GTD and Early Pregnant GTD Patients
10.4.2 Prior History of GTN and Early Pregnant GTN Patient
10.4.3 Twin Pregnancy with CHM
10.4.4 Contraception
10.4.5 Rare Presentations of GTN
10.5 Conclusions
References
Chapter 11 Female Genital Mutilation
11.1 Introduction
11.1.1 Definition
11.1.2 History
11.1.3 Why Is FGM Practised?
11.1.4 Incidence
11.2 Classification of FGM Types
11.2.1 Classification Challenges
11.2.1.1 Difficulties Associated with Classification of FGM
11.2.1.2 Differential Diagnosis
11.2.2 Some Useful Definitions
11.3 Health Complications of FGM
11.3.1 FGM and Psychological Consequences
11.4 Clinical Presentations
11.4.1 FGM Types 1 and 2
11.4.2 FGM Type 3
11.4.3 Deinfibulation
11.4.4 FGM Type 4
11.5 Management of Pregnant Women Presenting to a Maternity Setting
11.5.1 Obstetric and Neonatal Risks Associated with FGM
11.5.2 A Holistic Best Practice Consultation Should Include:
11.6 Management of Pregnant Women with Type 3 FGM
11.6.1 Antenatal Deinfibulation
11.6.2 Intrapartum Deinfibulation
11.7 Safeguarding and Law
11.8 Conclusion
References
Chapter 12 Ovarian and Cervical Malignancy in Pregnancy
12.1 Background
12.2 General Principles of Managing Cancer in Pregnancy
12.3 Cervical Cancer
12.3.1 Pre-Malignant Cervical Conditions
12.3.2 Previous History of Cervical Malignancy
12.3.2.1 Antepartum Management
Women with a history of simple excisional treatment such as LLETZ
Women with a history of trachelectomy
12.3.2.2 Intrapartum Management
Women with a history of simple excisional treatment such as LLETZ
Women with a history of trachelectomy
12.3.2.3 Post-Partum Management
12.3.3 Cervical Cancer in Pregnancy
12.3.3.1 Symptoms and Diagnosis
12.3.3.2 Staging of Cervical Cancer in Pregnancy
12.3.3.3 Principles of Management of Cervical Cancer in Pregnancy
12.3.3.4 Definitive Treatment
12.4 Ovarian Cancer
12.4.1 Previous History of Ovarian Malignancy
12.4.2 Adnexal Mass Presenting in Pregnancy
12.4.3 Suspected Borderline Ovarian Tumours in Pregnancy
12.4.4 Suspected Ovarian Malignancy in Pregnancy
References
Chapter 13 Post-Partum Contraception
13.1 Background
13.2 Antenatal Planning for Post-Partum Contraception
13.2.1 When to Have the Discussion
13.2.2 How to Have the Discussion
13.2.3 What to Offer
13.3 Methods of Contraception
13.4 UK Medical Eligibility Criteria (UKMEC)
13.5 Overview of Contraceptive Method Use in the Post-Partum Period
13.5.1 Intra-Uterine Contraception (IUC)
13.5.2 Subdermal Implants (SDI)
13.5.3 Progesterone Only Injectables – Depo-Medroxyprogesterone Acetate (DMPA)
13.5.4 Combined Hormonal Contraception Including Oral, Vaginal and Transdermal Preparations
13.5.5 Progestogen Only Pills (POP)
13.5.6 Lactational Amenorrhoea Method (LAM)
13.5.7 Barrier Methods
13.5.8 Fertility Awareness Methods (FAM)
13.6 Breastfeeding and Contraception
13.7 Initiating Post-Partum Contraception
13.7.1 How Soon Can Contraception be Initiated Post-Partum?
13.7.2 Additional UKMEC Conditions
13.8 Emergency Contraception in the Post-Partum Period
13.9 Service Considerations
References
Further Sources of Information on Individual Contraceptive Methods
Chapter 14 Pregnancy Associated Breast Cancer
14.1 Epidemiology of Pregnancy Associated Breast Cancer
14.1.1 Stage at Diagnosis
14.1.2 Disease Biology
14.1.3 Prognosis
14.1.4 Risk Factors
14.2 Diagnosis
14.2.1 Pregnancy Termination
14.2.2 Obstetric Management
14.3 Treatment
14.3.1 Surgery
14.3.2 Systemic Chemotherapy and Radiotherapy
14.3.3 Endocrine Therapy
14.3.4 Radiotherapy
14.3.5 Future Fertility
14.4 Pregnancy in the Presence of Metastatic Breast Cancer
14.5 Conclusions
References
Index
| An aparitie | 31 July 2023 |
| Autor | Swati Jha, Priya Madhuvrata |
| Dimensiuni | 157 x 234 x 9 mm |
| Editura | Cambridge University Press |
| Format | Paperback |
| ISBN | 9781009208826 |
| Limba | Engleza |
| Nr pag | 180 |
-
1,58600 lei 1,50600 lei